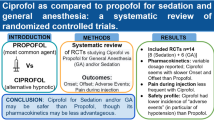
Summary
Abstract
Propofol (Diprivan®1) is a phenolic derivative with sedative and hypnotic properties but is unrelated to other sedative/hypnotic agents. Formulated as an oil-in-water emulsion for intravenous use, it is highly lipophilic and rapidly crosses the blood-brain barrier resulting in a rapid onset of action. Emergence from sedation is also rapid because of a fast redistribution into peripheral tissues and metabolic clearance. The depth of sedation increases in a dose-dependent manner.
In well designed clinical trials in patients receiving sedation in the intensive care unit (ICU) for a variety of indications, propofol provided adequate sedation for a similar proportion of time to midazolam, but the rate of recovery was faster with propofol. Even after periods of prolonged sedation (>72 hours), propofol was generally associated with a faster time to recovery than midazolam. Propofol facilitated better predictability of recovery and an improved control of the depth of sedation in response to titration than midazolam. In patients sedated following head trauma, propofol reduced or maintained intracranial pressure.
Propofol is associated with generally good haemodynamic stability but induces a dose-dependent decrease in blood pressure and heart rate. Bolus administration may cause transient hypotension, and slow initial infusions are recommended in most patients. Serum triglyceride concentrations should be monitored during prolonged infusions (>3 days) because of the risk of hypertriglyceridaemia. The administration of 2% propofol can reduce this risk. Strict aseptic technique must be used during the handling of the product to prevent accidental extrinsic microbial contamination.
Despite a higher acquisition cost with propofol, most studies of short-term sedation (approximately <3 days) showed that overall costs were lower with propofol than with midazolam, because a faster time to extubation reduced total ICU costs. However, as the period of sedation increased, the cost difference decreased.
Conclusion: The efficacy of propofol in the sedation of adults in the ICU is well established, and clinical trials have demonstrated a similar quality of sedation to midazolam. Because of a rapid distribution and clearance, the duration of action of propofol is short and recovery is rapid. Emergence from sedation is more rapid with propofol than with midazolam, even after long-term administration (>72 hours), which enables better control of the depth of sedation in response to titration and more predictable recovery times. Thus, for the ICU sedation of adults in a variety of clinical settings, propofol provides effective sedation with a more rapid and predictable emergence time than midazolam.
Pharmacodynamic Properties
Continuous infusions of propofol (Diprivan®) increase the depth of sedation in a dose-dependent manner. A good correlation generally exists between plasma propofol concentrations and the depth of sedation. The target plasma propofol concentrations identified to achieve a Ramsay sedation score of 2–5 ranged from 0.25 to 2.0 mg/L.
A rapid metabolic clearance and redistribution into peripheral tissues result in faster emergence from sedation than midazolam, even after prolonged periods of sedation (≥7 days). The emergence from propofol sedation is dependent on the depth of sedation, the duration of sedation and the size of the patient.
Propofol causes a dose-dependent decrease in blood pressure as well as a less marked decrease in heart rate. Hypotension is greater with propofol than midazolam during administration of a bolus dose, but similar to midazolam during continuous infusions. The mean heart rate associated with propofol sedation is generally lower than that associated with midazolam. Propofol decreases total oxygen consumption to a similar extent to midazolam. Right ventricular ejection fraction was improved in patients with acute respiratory failure sedated with propofol. Propofol sedation is associated with slight respiratory depression.
Following head injury, sedation with propofol maintained or decreased intracranial pressure and, in most cases, mean cerebral perfusion pressure was maintained above the target value of 60mm Hg.
Long-term infusions of propofol (>7 days) may cause increases in serum triglyceride concentrations. When prolonged sedation is indicated, 2% propofol provides the advantage of less lipid administration and, therefore, less hypertriglyceridaemia.
Propofol containing the bacteriostatic agent disodium edetate (ethylene-diaminetetraacetic acid [EDTA]) did not alter calcium and magnesium homeostasis or renal function in critically ill patients in a variety of medical and surgical intensive care unit (ICU) settings.
Pharmacokinetic Properties
Propofol is highly lipophilic facilitating rapid penetration of the blood-brain barrier and a fast onset of action (usually within 40 seconds). The pharmacokinetic properties are characterised by a three-compartmental model: rapid initial distribution from blood into tissues, rapid redistribution and metabolic clearance, and a slow return from poorly perfused tissues into the bloodstream. The rapid redistribution into peripheral tissues (muscles and fat) and the rapid metabolic clearance result in a short duration of action (approximate half-life 30–60 minutes) and a fast emergence from sedation when the infusion is stopped (usually within 10–15 minutes).
Propofol has a linear pharmacokinetic profile. At steady state, the clearance of propofol is dependent on metabolism and distribution to peripheral tissues. The volume of distribution is large and increases as the duration of the infusion increases, but once peripheral compartments become saturated, the distributional component of clearance decreases. In obese patients, a greater accumulation in the fatty tissues can cause slower clearance. The total body clearance of propofol ranges from approximately 96 to 204 L/h (23–50 mL/kg/min) and exceeds hepatic blood flow, indicating some form of extrahepatic metabolism. Propofol is extensively metabolised and excreted in the urine (≥88%), mainly as inactive metabolites.
In elderly patients, the volume of distribution and clearance of propofol is decreased and a lower dosage is required. In patients with renal and hepatic impairment, propofol anaesthesia did not significantly affect the pharmacokinetic parameters compared with patients with normal hepatic and renal function, but the effects of long-term sedation have not been evaluated in this patient group.
Clinical Efficacy
In well designed clinical trials in adult patients requiring ICU sedation in various clinical settings (including following cardiac surgery), propofol provided a similar quality of sedation to midazolam but was associated with a faster rate of recovery.
In patients sedated for general medical conditions, trauma or following general surgery, propofol provided a similar quality of sedation to midazolam, lorazepam, dexmedetomidine and isoflurane. Propofol infusions administered for varying periods at mean infusion rates of 1.62–2.8 mg/kg/h provided adequate sedation for 62–97% of the time compared with 57–93% of the time with midazolam (0.04–0.2 mg/kg/h). In studies of patients receiving short- (≤24 hours), medium- (24–72 hours) or long-term (>72 hours) sedation, patients treated with propofol generally awoke more rapidly and with less variability than those treated with midazolam. For example, in a study of critically ill patients sedated for approximately 80 hours, those treated with propofol had a mean time to recovery of 23 minutes versus 137 minutes in the midazolam group (p < 0.05). Even after receiving sedative infusions for >7 days, propofol was associated with a faster time to recovery than midazolam. The control of the depth of sedation was easier with propofol than with midazolam, since patients receiving propofol responded more quickly to changes in the infusion rate.
After undergoing cardiac surgery, propofol provided patients with a similar or improved quality of sedation to midazolam. Compared with midazolam, propofol was associated with a faster mean time to spontaneous ventilation (66–197.8 vs 13.6–52 minutes, respectively) and, overall, a faster mean time to extubation.
Propofol provides good control of cerebral haemodynamics in patients sedated following head trauma or neurosurgery. In patients with head injuries, propofol controlled intracranial pressure as effectively as fentanyl or pentobarbital plus morphine and appeared more effective than midazolam plus morphine.
Tolerability
Propofol has a cardiovascular depressant effect, which can lead to hypotension (incidence of 26%) and a reduced heart rate. In particular, bolus doses of propofol are associated with marked transient hypotension. Care should be taken in the elderly and in patients who are haemodynamically unstable or hypovolaemic.
The lipid emulsion of the propofol formulation provides an excellent medium for the growth of a variety of organisms. To prevent accidental extrinsic microbial contamination, strict aseptic technique must be used during handling of both the original formulation and that containing the bacteriostatic agent EDTA.
Pain on injection is common with propofol when administered into peripheral veins, but it can be reduced by using the larger veins in the forearm. Hypertriglyceridaemia is associated with propofol infusions of >3 days. Other adverse effects associated with propofol include respiratory acidosis during weaning from the ventilator (3–10%), green discolouration of the urine and the rare occurrence of anaphylactoid reactions. Case reports have suggested the risk of a possible propofol-infusion syndrome leading to myocardial failure and death in some patients receiving long-term (>58 hours), high-dose (>5 mg/kg/h) infusions.
Pharmacoeconomic Considerations
Despite the higher acquisition cost of propofol, pharmacoeconomic studies have generally shown a cost advantage for propofol compared with midazolam, due to faster recovery times leading to reduced total ICU costs.
In patients requiring sedation for at least 12 hours, the total cost per patient for a stay in ICU was about two-thirds less for patients treated with propofol plus alfentanil compared with patients treated with midazolam plus morphine (£3 095 vs £9 511; p = 0.0013). In a study of patients receiving long-term sedation (≈5.5 days) with propofol (1–6 mg/kg/h) or midazolam (0.1–0.5 mg/kg/h), a total ICU cost difference of $US1 362 per patient was found in favour of propofol. Costs included drug costs ($US0.026/mg for propofol and $US0.123/mg for midazolam) and costs incurred during sedation and weaning periods.
A sensitivity analysis based on a hypothetical model developed from a well designed study of patients sedated for periods of approximately 16 hours predicted a potential saving with propofol of between $Can244 and $Can570 (1997 dollars) for each ICU patient compared with midazolam. This saving was due to the shorter time to extubation leading to improved discharge planning. Extubation time with propofol appeared to be 4.2 times faster, and drug costs 3.6 times higher, than with midazolam.
Overall, studies have shown that the cost differential between propofol and midazolam reduces as the period of sedation increases. During short-term sedation (<24 hours in one study and <72 hours in another) propofol had a significant cost advantage over midazolam, but for longer periods of sedation (>72 hours), the higher acquisition cost of propofol offset the savings made from the reduced time in ICU.
Dosage and Administration
Propofol intravenous injectable infusions should be initiated slowly at a dosage of 0.3 mg/kg/h and adjusted upwards, as clinically indicated, in increments of 0.3–0.6 mg/kg/h at intervals of at least 5 minutes. A rate of between 0.3 and 3.0 mg/kg/h should achieve satisfactory sedation in most patients. Elderly patients (>55 years) require a reduced rate of infusion (1.8 mg/kg/h).
There is large interpatient variability in dosage requirements, which may change over time. Titration of the propofol dosage should be made to clinical response, and daily assessment of sedation levels and CNS function are important to determine the minimum dosage required. Bolus doses of 1% propofol may be given if clinically indicated and if hypotension is not likely to occur. A light level of sedation is recommended during the weaning process with discontinuation of the infusion 10–15 minutes before extubation.
Similar content being viewed by others
1. Introduction
Propofol (Diprivan®) is an established intravenous anaesthetic agent that gained US FDA approval for the sedation of mechanically ventilated adults in the intensive care unit (ICU) in 1993. Extensive clinical experience in ICU sedation in a variety of clinical settings now exists, and much of this was previously reviewed in Drugs.[1] This review focuses solely on the use of propofol for ICU sedation and expands on the clinical knowledge of the formulation gained since that time. Pharmacological data taken from studies of propofol given for indications other than sedation have also been included. Although generic formulations of propofol have recently become available, the use of propofol throughout this review refers to Diprivan®. Unless stated otherwise, the discussion of propofol refers to the 1% (10 mg/mL) formulation.
2. Pharmacodynamic Properties
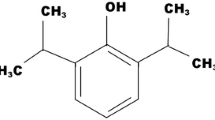
Propofol is a phenolic derivative (figure 1) formulated as an oil-in-water emulsion. It has sedative and hypnotic properties but is unrelated to other sedative/hypnotic agents.[2] In addition to the active compound, the formulation also contains soybean oil, glycerol, egg lecithin, sodium hydrochloride and water. To reduce the risk of infection, a formulation of propofol containing disodium edetate (ethylenediaminetetraacetic acid [EDTA]) [0.005% w/v], a bacteriostatic agent, is also available.[3] The main pharmacodynamic properties of the drug are summarised in table I.
2.1 Sedative Effects
Propofol is highly lipophilic and thus readily and rapidly crosses the blood-brain barrier resulting in a rapid onset of sedation.[4] The depth of sedation increased in a dose-dependent manner in healthy volunteers[5] and in patients after cardiac surgery,[6,7] and a correlation generally exists between plasma propofol concentrations and the level of sedation.[50] However, in one study of 22 patients sedated after coronary artery bypass graft (CABG) surgery, no correlation was found between plasma concentrations of propofol and depth of sedation, whereas a good correlation (r = 0.62) was found between the infusion rate and plasma concentration.[51]
Emergence from sedation after the propofol infusion is stopped is rapid as a result of the fast redistribution of the drug into peripheral tissues (section 3.1) and metabolic clearance (section 3.2). Emergence is faster following propofol sedation than after treatment with midazolam (sections 4.1.2 and 4.2), even after prolonged periods of sedation (≥7 days) [section 4.1.2]. A noncomparative study of 30 adult male patients (aged 21–80 years) requiring sedation for mechanical ventilation for >24 hours in a general medical and surgical ICU demonstrated that the emergence from propofol sedation is dependent on the depth of sedation, the duration of sedation (section 3.1) and the size of the patient (section 3.3.2).[21] Propofol was administered via a target controlled infusion (TCI) system, which is a computer-assisted infusion pump that controls the infusion rate to achieve and maintain a predetermined plasma concentration of the drug. Based on the pharmacokinetic profile of the drug in the first 20 study participants given propofol dosages based on short-term anaesthetic dosages, a pharmacokinetic-pharmacodynamic model for propofol sedation was developed and prospectively tested on the last ten patients.
The average steady-state infusion rate in the prospectively tested patients was 1.9 mg/kg/h, and all patients received intravenous or epidural infusions of fentanyl (≤200 µg/h) for analgesia as required.[21] The predicted propofol plasma concentrations required to induce modified Ramsay sedation scale scores of 2, 3, 4 and 5 (defined in table II) were 0.25, 0.6, 1.0 and 2.0 mg/L, respectively. The predicted emergence times after 24 and 72 hours and 7 and 14 days of light sedation (i.e. time taken for sedation score to decrease from 3 to 2) with propofol were 13, 34, 198 and 203 minutes, respectively, and after deep sedation (sedation score from 5 to 2), 25, 59, 71 and 74 hours. To facilitate emergence from light sedation, a 58% decrease in propofol plasma concentration was required, and for emergence from deep sedation, an 88% decrease was needed. The model predicted light and deep sedation with propofol with 73% accuracy.[21]
Ramsay sedation scale[53]
Similar target propofol plasma concentrations (range of 0.2–2.1 mg/L) were identified to achieve a desired level of sedation in a study using the Diprifusor ™ TCI system to sedate patients (≥18 years), requiring mechanical ventilation in the ICU.[22] The multicentre, noncomparative study included patients admitted for general medical or surgical care (n = 47) or after brain injury (n = 18) or cardiac surgery (n = 57). No significant differences between predicted and measured plasma concentrations were observed during sedation.[22]
Results of a further study also demonstrate the relationship between depth of sedation and propofol plasma concentration. To maintain a Ramsay sedation score of 2–3, the mean plasma concentration of propofol in critically ill patients (n = 10) was 0.58 mg/L, achieved by a mean infusion rate of 0.71 mg/kg/h.[52]
Although the mechanism has not been determined, coadministration of propofol and midazolam produces a synergistic sedative effect.[19] Mean maintenance dosages of both agents were reduced by 68% when they were coadministered to 25 patients after CABG surgery.[19] Synergistic hypnotic effects were observed in anaesthetic studies when propofol was combined with alfentanil, thiopental, midazolam or midazolam plus alfentanil, whereas an additive hypnotic effect was observed when propofol was coadministered with fentanyl (reviewed by Fulton and Sorkin[1] ).
2.2 Haemodynamic Effects
2.2.1 Effects on Blood Pressure and Heart Rate
Propofol causes a decrease in blood pressure, which is generally dose dependent[6,7,23] and thought to be due to a combination of decreased systemic vascular resistance and myocardial contractility.[54] In clinical practice, haemodynamic parameters are maintained within prescribed limits by the administration of inotropic drugs and intravenous fluids. Thus, in comparative studies, the hypotensive effect of propofol was not significantly different from that of midazolam during periods of continuous infusion (section 5.1). However, transient hypotension was associated with bolus doses of propofol in clinical trials (section 5.1).
After an initial bolus dose of propofol (1 mg/kg) or midazolam (0.07 mg/kg) was given to 30 patients following CABG surgery, mean arterial pressure (MAP) decreased by 15% (from 79.6 to 67.5mm Hg; p < 0.05) in the propofol group compared with 7% in the midazolam group (76.8 to 71.1mm Hg; not significant).[17] This initial decrease in MAP in patients receiving propofol lasted approximately 15 minutes, and after 1 hour of infusion, values stabilised at approximately 11% lower than baseline (figure 2), which was considered clinically acceptable. Cardiac output remained stable and there were no signs of myocardial ischaemia.[17]
The comparative effects of propofol and midazolam on mean arterial pressure and heart rate. Patients were randomised to a propofol loading dose of 1 mg/kg followed by a mean infusion rate of 2.7 mg/kg/h (n = 15) or a midazolam loading dose of 0.07 mg/kg followed by a mean infusion rate of 0.092 mg/kg/h (n = 15) after coronary artery bypass graft surgery.[17] * p < 0.05 vs comparator.
MAP and mean pulmonary arterial pressure decreased during propofol infusion, because of a reduction in systemic and pulmonary vascular resistance, in a study of 20 patients with acute respiratory failure requiring mechanical ventilation in the ICU.[55] The decrease in pulmonary arterial pressure led to an improved right ventricular ejection fraction (p < 0.01 vs pretreatment values).
In comparative studies of patients requiring sedation following cardiac surgery, the requirement for concomitant vasodilators (sodium nitroprusside or nitroglycerin) to treat postoperative hypertension was similar or reduced with propofol sedation compared with midazolam.[16–19,24,56]
Propofol causes a decrease in heart rate despite reducing MAP. Mean heart rate decreased significantly from baseline (p < 0.05) in 53 critically ill patients treated with propofol (mean infusion rate of 1.77 mg/kg/h), but not in those receiving midazolam (n = 47) [mean infusion rate of 0.10 mg/kg/h] for ≤24 hours in a general medical and surgical ICU.[8] In patients sedated after CABG surgery, the decrease in mean heart rate from baseline was not significant at any timepoint up to 6 hours from the start of the propofol infusion, whereas in the midazolam group, mean heart rate was significantly higher than baseline at hours 5 and 6 (p < 0.05).[17] Mean heart rate values at hours 4, 5 and 6 were significantly lower in patients receiving propofol than in those receiving midazolam (p < 0.05), and the difference increased over time (figure 2).[17]
In another study of patients sedated for approximately 14 hours after cardiac surgery, mean heart rate was significantly reduced from baseline in the 25 patients receiving propofol (from 110 to 93 beats per minute; p < 0.05), whereas patients receiving midazolam (n = 25) showed a slight increase in mean heart rate (from 106 to 112 beats per minute; nonsignificant difference).[19]
Recipients of dexmedetomidine sedation (median infusion rate of 0.00086 mg/kg/h; n = 10) had a significantly lower mean heart rate than propofol recipients (1–3 mg/kg/h; n = 10) during 8 hours of continuous infusion (p = 0.034); the study population consisted of postoperative patients requiring mechanical ventilation.[57] Respective mean heart rate values at baseline and at hour 8 were 94 and 91 beats/min for propofol and 92 and 72 beats/min for dexmedetomidine (values taken from graph). After discontinuation of the infusion, mean heart rate in the dexmedetomidine group returned to baseline values with no further difference between groups.[57]
Mean blood pressure appeared to be similarly affected by 1% or 2% propofol in one study,[58] but in another,[59] the effect on heart rate was different. In patients sedated for >48 hours after trauma (n = 63), mean blood pressure and heart rate were similar with 1% or 2% propofol or midazolam.[58] However, in patients sedated after cardiac surgery, 1% (n = 19) or 2% (n = 20) propofol had a similar effect on blood pressure, but mean heart rate was higher in the 2% propofol group during the period of 30–480 minutes (p = 0.006 from 1 to 4 hours). The reason for this observation is unknown.[59]
2.2.2 Effect on Oxygen Consumption
After cardiac bypass surgery, patients need to restore their normal body temperature. Rewarming is often associated with increased body oxygen consumption (VO2) and shivering, which places additional stress on the newly revascularised heart.[26] Propofol and midazolam were shown to reduce systemic VO2 to a similar extent in one randomised study of patients (n = 73) in a medical ICU.[27] However, in another randomised study of patients in the first 4 hours after cardiac surgery (or until rewarmed to 37°C), total body VO2 was reduced more in the group administered propofol 2 mg/kg/h (n = 12) than in the control group (n = 12) which received midazolam (dosage titrated to achieve a satisfactory level of sedation).[26] Total VO2 was measured using a pulmonary artery catheter. Median VO2 levels during rewarming were 1.8 L/h/m2 (30 mL/min/m2) less in the propofol group than in those receiving control (6.3 vs 8.1 L/h/m2 [105.2 vs 135.3 mL/min/m2]; p = 0.01). Shivering was also reduced in the group receiving propofol compared with the control group, however, this difference did not reach statistical significance. Patients receiving propofol were more heavily sedated (median Ramsay sedation score of 5) than those in the control group (median Ramsay sedation score of 3) [p = 0.001].[26]
In patients receiving light sedation after coronary artery surgery, low-dose propofol (1 mg/kg/h) plus diazepam as required (n = 15) was associated with slight haemodynamic suppression but did not decrease total-body VO2 compared with placebo plus diazepam (n = 15).[60] A dose-dependent effect on cardiopulmonary response to chest physical therapy was observed with propofol bolus infusions of 0.35 and 0.75 mg/kg administered 2 minutes before therapy.[61] Increases in VO2, oxygen delivery index and cardiac output were suppressed with both dosage groups, but effects were more marked with the higher dosage.
2.3 Respiratory Effects
Propofol has a slight, dose-dependent respiratory depressant effect, which has been reviewed previously.[28] Respiratory depression is not of concern in patients undergoing mechanical ventilation but is an important consideration during weaning from ventilation.[62] Because propofol is rapidly cleared from the blood (section 3.2), the respiratory depressant effect resolves quickly once the drug is stopped.[63]
Similar effects on respiratory parameters were observed during weaning from mechanical ventilation or after extubation in patients receiving propofol or midazolam in clinical trials,[14,18,24,25,56,64] with one exception.[20] In a study of 100 patients sedated after cardiac surgery, patients receiving midazolam (0.034 mg/kg/h; n = 50) had significantly higher mean arterial partial pressure of carbon dioxide (PaCO2) levels than patients receiving propofol (1.15 mg/kg/h; n = 50) [p < 0.001]. However, the significantly greater amounts of morphine administered to patients receiving midazolam (p < 0.001) may have accounted for this difference in PaCO2.[20]
Propofol was associated with rapid shallow spontaneous breathing in a noncomparative study of ten critically ill patients, but this effect on respiration resolved within 30 minutes of stopping the infusion.[65] The ratio of respiration rate to tidal volume determines the rapid shallow breathing index, which may be used to assess whether a patient is ready to be weaned from mechanical ventilation. Compared with 20–30 minutes after the propofol infusion was stopped, during treatment patients had a significantly lower tidal volume (0.342 vs 0.245L; p = 0.006) and higher RSBI (114.8 vs 155.6 breaths/min/L; p = 0.004). These results indicate that although propofol may cause rapid shallow breathing, this does not always mean that the patient is not ready to begin spontaneous ventilation.[65] This is less likely to be the case with benzodiazepines, particularly after prolonged sedation, because of the likelihood of prolonged respiratory depression after the infusion is stopped.[66]
A reduction in peak inspiratory pressure has been associated with propofol infusions, which suggests a mild bronchodilator effect.[29–31] In addition, propofol provided a good quality of sedation in patients with chronic obstructive pulmonary disease and facilitated a rapid recovery.[67]
2.4 Neurological Effects
2.4.1 Cerebral Haemodynamics and Metabolism
The dose-dependent effect of anaesthetic dosages of propofol on cerebral metabolism and decreased cerebral blood flow have been reviewed previously.[28] In patients with head injury receiving propofol for sedation during mechanical ventilation in the ICU, intracranial pressure (ICP) was either maintained or decreased[32–36] and, in most cases, mean cerebral perfusion pressure (CPP = MAP - ICP) was maintained above the target value of 60mm Hg.[32–34] In one study (n = 31), a further subgroup analysis demonstrated that the decrease in ICP was significant in patients with a high (>16mm Hg) baseline ICP (p < 0.05) and was unchanged in patients with low (≤16mm Hg) baseline ICP.[35]
After severe head injury, a decrease in ICP was not observed in 15 patients receiving a mean propofol dosage of 232 mg/h.[68] However, propofol was associated with a transient decrease in global brain metabolism, which was reduced 4 hours after the start of the infusion but returned to presedation values at 8 hours.[68]
Propofol improved cerebral autoregulation after head injury in a study of eight patients admitted to the ICU.[69] Autoregulation was tested three times in each patient: during midazolam and fentanyl sedation, during sedation with propofol 6 mg/kg/h and during sedation with propofol 12 mg/kg/h. The index of autoregulation (IOR) was defined as the ratio of the percent change in the estimated cerebral vascular resistance to the percent change in the MAP. Preliminary results, presented in an abstract, demonstrate that the IOR was significantly improved with administration of propofol 12 mg/kg/h (IOR = 0.99; p < 0.05) but was not improved in the other treatment groups.[69]
2.4.2 Effects on the EEG
During conscious sedation, propofol has been associated with a dose-dependent increase in the activation of the electroencephalogram (EEG), primarily in the β1-frequency range (as reviewed by Kishimoto et al.[70] ). EEG derivatives, such as the bispectral index, have been used to assess brain wave activity to determine the depth of sedation.[71]
Computer-controlled infusions of propofol to achieve target plasma concentrations of 0.3, 0.6, 0.9 and 1.2 mg/L for a median duration of 87 minutes produced a progressive increase in mean reaction times as well as a progressive decrease in the long latency cognitive P300 auditory evoked response.[72] However, more recent evidence suggests a nonlinear relationship between electrocortical activity and depth of sedation during a longer period of constant sedation (>12 hours).[71] Administration of propofol 1–4 mg/kg/h for >12 hours was associated with a decrease in EEG frequency.[71] Because of this time-dependent deceleration in EEG frequency, EEG parameters should be used cautiously to monitor the depth of ICU sedation over the longer term.[71]
2.4.3 Other Neurological Effects
Data regarding the analgesic properties of propofol are equivocal (reviewed by Fulton and Sorkin[1] ), and other reviews suggest that at sedative dosages, propofol has no analgesic effects.[63,73] Adequate pain relief in critically ill patients is usually achieved with opioid analgesics, which will decrease the overall requirement for sedation.[63] Compared with patients receiving midazolam after cardiac surgery, patients treated with propofol had lower[16,20,24] or similar[17–19,56] requirements for analgesia during ICU sedation. However, patients sedated with propofol (n = 10) required 3-fold more alfentanil than those receiving dexmedetomidine (n = 10) in one randomised study (p = 0.004).[57] Propofol has a slight amnesic effect, but less than that observed with the benzodiazepines.[54]
In some patients requiring sedation for >7 days, there have been reports of a need for an increasing dosage of propofol because of the development of tolerance.[37,38] In a noncomparative study designed to evaluate the development of tolerance in patients sedated with propofol (approximate dosage of 0.5–4.0 mg/kg/h) for >5 days, 3 of 11 patients were considered to demonstrate tolerance because of a statistically significant increase in both the infusion rate and blood concentration of propofol (p < 0.05).[39] These results indicate a possible need for increasing the dosage in some patients who require long-term sedation.
Sleep deprivation can exacerbate emotional stress in critically ill patients in the ICU.[74] A diurnal sleep-wake cycle was achieved in most critically ill patients (n = 29) receiving additional night sedation (ANS) with 2% propofol alternating with constant light sedation (CLS) with 2% propofol during the day.[75] Patients were randomised to receive 50 hours of CLS day and night (n = 15) or alternating light sedation with ANS (n = 15). The propofol infusion rate was titrated based on the Ramsay scale (defined in table II), with a target Ramsay score of 2–3 for light sedation and a target score of 4–5 for ANS. Morphine was also administered as required. A significantly improved rhythm of sedation levels was observed in the group receiving ANS compared with those receiving CLS (p < 0.01). The mean propofol infusion rate in the CLS group was 1.01 mg/kg/h during the day and 0.97 mg/kg/h at night, and in the ANS group respective propofol day and night infusion rates were 0.56 and 0.94 mg/kg/h. ICU patients least likely to exhibit a diurnal sedation pattern in response to ANS were those who were well enough to establish normal diurnal fluctuations and those who were severely ill with obtunded consciousness.[75]
Sleep quality improved to a similar extent in patients receiving propofol (n = 19) or midazolam (n = 13) in a study evaluating overnight sedation of non-intubated conscious patients admitted to ICU following trauma or general surgery.[74] However, this did not appear to affect the level of anxiety and depression, which was considered high in both treatment groups in the first 5 days in the ICU.[74]
Amnesia has been reported to occur in a dose-dependent fashion with the administration of propofol anaesthesia (reviewed by Fulton and Sorkin[1] ). However, propofol caused less amnesia than midazolam in critically ill patients[14] and healthy volunteers[76] at dosages that produced similar sedative effects.
2.5 Effects on Lipid Metabolism
As a result of the lipid content of propofol, long-term infusions (>3 days) have been associated with progressive increases in serum triglycerides (section 5.4).[9,40,41] In addition, the acute-phase response following major stress in critically ill patients can have an effect on lipid metabolism, lowering serum cholesterol and raising triglycerides.[42]
Propofol infusions of >7 days (mean maintenance dosage of 2.31 mg/kg/h) caused 3 to 4-fold increases in serum triglyceride concentrations, and the return to presedation values was variable, in some instances taking several days.[40]
When more prolonged sedation is indicated, the administration of 2% propofol reduces the lipid content of the dosage by half and, therefore, causes less hypertriglyceridaemia (section 5.4). In a study of 30 critically ill patients sedated with 2% propofol for >50 hours, serum triglyceride concentrations were not significantly increased.[42] A significant correlation between C-reactive protein and triglycerides (p < 0.01) was observed, however, indicating that the acute-phase response may have had some effect on the mild increases in serum triglyceride concentrations.[42] Similarly, the frequency of hypertriglyceridaemia was reduced in patients sedated with 2% propofol (n = 51) for a mean duration of 122.4 hours compared with historical data of patients receiving 1% propofol (3.9 vs 20.4%, respectively; p = 0.016).[43]
In a further study, the effects on plasma total cholesterol and triglyceride levels observed with 1% and 2% propofol were not significantly different.[77] In this randomised, multicentre, nonblind study of patients requiring mechanical ventilation in the ICU, infusion rates of propofol were similar in both the 1% and 2% treatment groups, and the mean duration of sedation was 58 and 55 hours, respectively (n = 28 in both groups).[77] Higher cholesterol and triglyceride concentrations were observed in patients receiving 1% propofol on days 1 and 2, but on day 3, triglyceride concentrations were higher in patients receiving 2% propofol. The differences between the groups did not reach statistical significance. Triglyceride concentrations were raised to above the upper normal limit (1.6–1.92 mmol/L) in three patients in the 1% group and in one patient in the 2% group.[77]
Pancreatic dysfunction, resulting from raised serum triglycerides, has been associated with prolonged propofol administration.[78–81] A randomised study compared the effects of postoperative sedation with propofol (n = 21) or midazolam (n = 21) on pancreatic function.[82] Four hours after the start of sedation in the ICU, mean serum triglyceride concentrations were within normal limits but were significantly higher in the propofol group (1.58 mmol/L) than in the midazolam group (0.92 mmol/L) [p < 0.05]. However, there were no significant differences between treatment groups in the serum concentrations of markers of pancreatic function (amylase, lipase and pancreatic-associated protein), and all were inside the normal range. These results suggest that pancreatic function may not be altered with sedative dosages of propofol administered postoperatively.[82]
2.6 Effects on Endocrine Response
Propofol sedation is associated with decreases in mean serum cortisol concentrations.[8,24] This effect is most likely attributable to the sedative effect of propofol mitigating sympathetic activity in response to stress in critically ill patients, thereby minimising catecholamine release.[44]
The effect of propofol on the postoperative endocrine response was evaluated in patients after undergoing CABG surgery in a randomised study.[44] Patients received a continuous infusion of propofol (n = 61) or intermittent bolus doses of midazolam and morphine (n = 60) to maintain a sedation level of 5 on a modified Ramsay sedation scale. Compared with patients receiving midazolam, propofol recipients had a 31% lower plasma cortisol concentration (p = 0.0004) and a 53% lower plasma adrenaline (epinephrine) concentration (p = 0.009) 8 hours after admission to the ICU. Although the study was not designed to correlate haemodynamic changes with the endocrine response, a lower incidence of tachycardia (p = 0.038) and hypertension (p = 0.012) and an increased incidence of hypotension (p = 0.001) were observed in the propofol group than in the midazolam group. Plasma noradrenaline (norepinephrine) concentrations were also lower in the propofol group at 8 hours, but the difference did not reach statistical significance. The effect on plasma dopamine concentrations was similar in both treatment groups. In the period 6–12 hours after admission to the ICU, mean urinary concentrations of cortisol, dopamine, adrenaline and noradrenaline were significantly lower in the propofol group than in the midazolam group (p ≤ 0.01).[44]
In a further study of sedation after uncomplicated CABG surgery, patients receiving light sedation with propofol (Ramsay score of 2) [n = 24] did not have an increased endocrine stress response or risk of myocardial ischaemia compared with patients receiving heavy sedation with propofol (Ramsay sedation score of 4) [n = 26].[83] In a subgroup of patients, mean plasma concentrations of adrenaline, noradrenaline and dopamine were not significantly different in light (n = 11) and heavy (n = 10) sedation groups up to 24 hours after surgery.
Increasing the dosage of propofol for overnight sedation did not restore hormonal diurnal rhythms.[84] There were no significant effects on mean serum concentrations of cortisol, growth hormone, adrenocorticotrophic hormone, prolactin or thyroid stimulating hormone in 30 critically ill patients maintained at a level of light sedation or those receiving additional night sedation with either a variable infusion of 2% propofol or a constant infusion of morphine and 2% propofol (results presented in an abstract).[84]
2.7 Other Effects
2.7.1 Effect on Gastrointestinal Motility
In vitro, clinically relevant dosages of propofol impaired spontaneous contractile activity and acetylcholine-induced contraction of human gastric and colonic smooth muscles.[85] However, there was no difference in gastro-caecal transit times in patients anaesthetised with propofol (119 minutes), propofol/ketamine (147 minutes) or isoflurane (122 minutes), indicating that in the ICU setting, propofol is not likely to alter gut motility more than standard isoflurane anaesthesia.[86]
2.7.2 Effects on the Immune System
Anaesthetic agents are known to effect the immune system.[49] In vitro studies have shown that propofol, and other anaesthetic/sedative agents, effect lymphocyte response,[48,87] neutrophil function[46,47,88] and cytokine production.[89] Although these effects are generally reversible after short-term anaesthetic use, they may be clinically relevant for the sedation of immunocompromised patients or patients undergoing prolonged sedation in the ICU.[49] In the case of propofol, the lipid emulsion may cause an immunosuppressive effect.[48,49]
After 48 hours of continuous infusion, serum concentrations of pro-inflammatory cytokines (interleukin [IL]-1β, IL-6 and tumour necrosis factor-α), which act to limit infection and provide a suitable environment for tissue healing, were increased significantly in surgical patients receiving propofol (p < 0.05), but decreased significantly in patients receiving midazolam (p < 0.05).[90] The production of IL-8 was reduced significantly by both propofol (30%) and midazolam (48%) [p < 0.05 vs preinfusion levels]. Production of the immunoregulatory cytokines was also affected; IL-2 production was reduced by propofol (68%; p < 0.001), and interferon-γ production was increased by propofol (30%; p < 0.05), whereas midazolam did not cause a significant change in either parameter.[90]
2.8 Effects of Propofol Containing Disodium Edetate
To inhibit microbial growth, propofol is also available in a formulation containing EDTA. As well as its bacteriostatic effect, EDTA is a chelator of ions (e.g. calcium and magnesium) and trace metals (e.g. zinc and copper). Various well-designed studies have compared the effects of propofol, with and without EDTA, in critically ill patients.[91–95]
The addition of EDTA to propofol does not alter calcium and magnesium homeostasis or renal function in critically ill patients with pulmonary dysfunction[91] or following general[92] or cardiac[92,93] surgery. Compared with propofol without EDTA, propofol containing EDTA was associated with a greater loss of zinc and iron in the urine and lower serum concentrations of zinc, but the clinical relevance of this is not clear.[94]
Propofol with and without EDTA was shown to increase concentrations of parathyroid hormone in healthy volunteers[95] and patients with pulmonary dysfunction.[91] The reasons for this increase and the clinical relevance are unclear.[95]
3. Pharmacokinetic Properties
The pharmacokinetic properties of propofol are characterised by a three-compartmental model: rapid initial distribution from blood into tissues, rapid redistribution and metabolic clearance, and slow return from poorly perfused tissues into the blood.[4] The rapid occurrence of the first two phases of this model results in a fast onset of action (usually within 40 seconds) and a rapid rate of recovery from sedation (usually within 10–15 minutes).[3]
The pharmacokinetic properties of propofol have been well described previously.[96] This section includes more recent studies of propofol in patients and healthy volunteers. Table III summarises the mean distribution and elimination pharmacokinetic parameters observed in patients receiving short-term (≤24 hours) or long-term (72–86 hours) sedation with propofol in the ICU.
3.1 Blood Concentrations and Distribution
After the initial dose-dependent increase in blood propofol concentrations, the rate of increase slows as a result of rapid distribution and the high rate of metabolic clearance.[3] During continuous infusions of propofol used as an anaesthetic or for ICU sedation, blood concentrations at steady state are linearly related to the infusion rate.[100] Mean whole-blood concentrations of propofol after a bolus dose of 1–3 mg/kg (n = 9) ranged from 0.77 to 15.3 mg/L, and 6 hours after a subsequent continuous infusion of 3 mg/kg/h, the mean blood propofol concentration was 1.3 mg/L. Thereafter, blood propofol concentrations gradually increased to reach a plateau of approximately 2 mg/L at about hour 30, which was maintained until the infusion was stopped (hour 72).[98]
Because propofol is highly lipophilic, it readily crosses the blood-brain barrier.[101] The drug is also extensively distributed into other well perfused tissues, then to lean muscle tissue and finally into fat.[101] The manufacturer’s prescribing information states that the initial distribution half-life ranges from 2 to 4 minutes, followed by a rapid redistribution into poorly perfused tissue (elimination half-life [t1/2β] 30–60 minutes).[101] Individual pharmacokinetic studies recorded an t1/2β of 70.9[99] and 90.5[97] minutes (table III). The final phase is characterised by a slow redistribution from poorly perfused tissue.[101]
The large volume of distribution of propofol is greater during long-term sedation than during short-term infusions.[97] After major surgery or trauma, 18 patients were sedated with propofol via a TCI system (plus alfentanil for analgesia) for up to 24 hours (mean duration 19 hours). The volume of distribution at steady state (Vss), assuming a mean bodyweight of 70kg, was 7 L/kg, and about 2-fold higher than that observed during studies of short-term propofol infusions for anaesthesia.[97] Another study in patients receiving propofol sedation over 72 hours estimated a larger mean Vss of 23.8 L/kg (table III),[98] and for infusions of 10 days, the value approached 60 L/kg.[3] The observed increase in Vss values over time probably reflects increased peripheral distribution compared with short-term infusions.
Propofol is highly protein bound (98–99%).[102] A decrease in concentrations of serum albumin in critically ill patients can lead to an increase in the percentage of free propofol, but the clinical significance of this is not clear.[102]
3.2 Metabolism and Elimination
Following an initial bolus dose of propofol, plasma concentrations rapidly decrease as a result of rapid distribution and high metabolic clearance, each accounting for approximately half of the decrease.[3] Over time, there is a reduction in the distribution of the drug as the concentration in body tissues equilibrates with that in plasma. At this stage, there is no longer a transfer between tissues and plasma, and therefore concentrations fall more slowly when the infusion is stopped.[3]
According to the manufacturer’s prescribing information, the total body clearance (CL) of propofol ranges from 96 to 204 L/h (23–50 mL/kg/min) in 70kg adults[3] and exceeds hepatic blood flow, indicating some form of extrahepatic metabolism.[96] Individual pharmacokinetic studies recorded a CL of 60 L/h for infusions of ≤24 hours[97] and 94.2[98] and 126.6[99] L/h for infusions of 72–86 hours (table III). Elimination is mainly via hepatic conjugation to inactive metabolites, which are excreted via the kidney.[3] Less than 0.3% of unchanged propofol was excreted in the urine after administration of [14C]propofol (mean dose 0.47 mg/kg) in healthy volunteers.[103] Most of the drug was excreted in the urine (≥88%) as inactive glucuronide conjugates of propofol with the corresponding quinol and the 4-sulphate conjugate of the quinol.[103]
The terminal elimination half-life (t1/2γ) of propofol is characterised by the slow return of the drug from poorly perfused tissue (mainly fat) back into the bloodstream. Studies of patients receiving long-term infusions (up to several days) of propofol for sedation in the ICU demonstrate a t1/2γ of 23.5[99] and 31.3 hours.[98] Nevertheless, this long elimination phase appears to be of little clinical significance, as rapid clearance from the plasma results in rapid emergence from sedation once the infusion is stopped,[63] and recovery has been shown to be rapid even after long periods of infusion in several clinical trials (section 4.1.2 and 4.2). However, with higher than recommended dosages and long-term infusions, the return of propofol from the peripheral tissues into the plasma will slow recovery after the infusion is stopped.[3] Thus, to avoid excess drug accumulation during long-term infusions, the dosage should be titrated to achieve clinical response (section 7).[3]
The temporary increase in hepatic blood flow that occurs after eating may affect the pharmacokinetic behaviour of some drugs.[104] Switching from parenteral to enteral feeding in eight patients receiving long-term sedation with propofol in the ICU did not affect hepatic blood flow or systemic clearance of the drug.[104]
3.3 Special Populations
3.3.1 Elderly Patients
In elderly patients, the volume of distribution and clearance of propofol is decreased and a lower dosage is required (section 7).[3] In patients aged 65–80 years (n = 12), the volume of distribution of propofol for the central compartment was 0.32 L/kg compared with 0.40 L/kg in patients aged 18–35 years (n = 12).[105] The reduced volume of distribution is a result of a lower cardiac output in elderly patients, leading to a reduced perfusion of tissue relative to body mass.[105] Clearance was reduced by 28% in patients aged >60 years compared with those aged <60 years after receiving an infusion of propofol.[106]
3.3.2 Obese Patients
In obese patients, the volume of distribution is increased but the clearance is slower than that observed in lean patients.[21] This is due to increased saturation and drug accumulation in the fatty tissue of obese patients, especially after long-term infusions.[21] When the propofol infusion is discontinued in this patient group, the rate of the decrease of the plasma propofol concentration becomes less dependent on redistribution and more dependent on metabolic clearance.[21] A slower rate of decrease of plasma propofol concentrations results, and potentially increases the emergence time of obese patients.[21] In a study of propofol dosage regimens, the pharmacokinetics of the drug were best described when covariates of lean and fat body masses were added to the standard three-compartment model (section 2.1).[21] In this study, the estimated Vss for a mean infusion of 55 hours (n = 19) was almost 3-fold greater than a previous estimate using a noncompartmental model in patients sedated with propofol for 72 hours (n = 9) [65 vs 23.8 L/kg].[21] Similarly, the t1/2γ value was also increased in the study using a three-compartmental model and including covariates of body mass compared with the study using a noncompartmental model (50.3 vs 31.3 hours).[21] Basing the propofol dosage on the ideal bodyweight, rather than the actual bodyweight of morbidly obese patients, should prevent significant drug accumulation and oversedation.[21]
3.3.3 Patients with Renal or Hepatic Impairment
The pharmacokinetic parameters of propofol anaesthesia in patients with chronic hepatic or renal impairment are not significantly different from patients with normal hepatic and renal function,[96] but the effects of long-term propofol sedation have not been evaluated in these patient groups. In a study of patients with established renal failure receiving sedation with propofol and undergoing haemodiafiltration, the requirement for propofol was not affected but plasma propofol concentrations were reduced with the initiation of the extracorporeal circuit.[107] The pharmacokinetics of propofol have not been determined in patients with acute renal or hepatic failure.[3]
Cation homeostasis and renal function were not adversely affected by propofol containing EDTA in patients with chronic renal impairment.[108] The effect of propofol with EDTA on renal function was similar to the effect of propofol without EDTA in a double-blind, multicentre study.[108]
3.4 Drug Interactions
The sedative effects of propofol may be increased when coadministered with intramuscular or intravenous narcotics (e.g. morphine and fentanyl), and a more profound reduction in blood pressure and cardiac output may occur.[3] In adults, there have been no significant interactions with propofol and other commonly used neuromuscular blocking agents, muscle relaxants and analgesic agents.[3]
Propofol undergoes hydroxylation via the cytochrome P450 (CYP) 2C9 pathway, and systemic clearance may have some dependence on CYP2C9 activity.[109] When propofol was coadministered with parecoxib, a parenteral cyclo-oxygenase-2 specific inhibitor and prodrug to a substrate for hepatic CYP2C9, there were no significant differences in pharmacokinetic parameters compared with propofol administered in combination with placebo.[109]
4. Clinical Efficacy
The efficacy of propofol as sedation for adult patients in the ICU has been assessed in numerous fully published studies in a range of patient populations. This section focuses primarily on randomised, comparative trials, many of which were nonblind because the propofol formulation is readily distinguishable, and knowledge of treatment groups could be an advantage in the management of acute agitation.[64] The number of evaluable patients in each study ranged from approximately 20 to 100, with some of the larger studies recruiting patients from several ICUs. In most cases, analyses were intention-to-treat. Efficacy parameters included assessment of the time spent with adequate sedation, which in most cases was measured by using the Ramsay sedation scale (table II) or a modified version. Recovery from sedation was assessed by a variety of measures, including time to answer questions, time to achieve level 3 on the Ramsay sedation scale and time to ventilator weaning and extubation (see table IV). The time to extubation and/or recovery varies greatly between studies, largely because of the varying practices between ICUs and the different measures used to assess recovery times. In addition, between studies there was variation in the depth of sedation at which patients were maintained and diagnoses of patients. In studies of patients with neurological conditions, the sedative effect on intracranial pressure and cranial perfusion pressure was also assessed (section 4.3).
Efficacy of propofol (PRO) for sedation of patients requiring mechanical ventilation in the intensive care unit. Summary of randomised, comparative, nonblind trials in patients with general medical conditions, with trauma or following general surgery. Trials were single-centre studies except for one[8]
Patients enrolled in all studies were aged between 16 and 80 years. Sedative agents were administered intravenously, in most cases via a central line. If clinically indicated, a bolus dose of sedative was given initially; thereafter the sedative was given as an infusion and the rate was titrated to achieve a desired level of sedation. This method of variable-rate infusion reduces the risk of oversedation (section 3.2). Dose-finding studies in patients receiving sedation after cardiac surgery showed that, in general, lower dosages of propofol (<0.75 mg/kg/h) resulted in a greater need for supplementary sedation or for analgesics, whereas higher dosages (≥1.5 mg/kg/h) were associated with oversedation and hypotension.[6,7,112,113] Patients were excluded if they were pregnant, were grossly obese or had a known allergy to the study medications. Treatment groups within studies were generally well matched in terms of age, weight and severity of condition.
4.1 Sedation For Medical Conditions, Trauma and Following General Surgery
The efficacy of propofol in the sedation of critically ill patients with various medical conditions or following trauma or general surgery, has been compared with midazolam,[8–15,37,41,64] midazolam or lorazepam,[110] dexmedetomidine[57] and isoflurane.[111] Results are summarised in table IV.
Studies included patients who were expected to need mechanical ventilation for periods ranging from approximately 8 hours to >7 days. In most cases, an opioid analgesic was administered concomitantly with sedation, and the use of neuromuscular blocking agents was generally limited to facilitate tracheal intubation.
4.1.1 Quality of Sedation
Overall, in randomised studies directly comparing propofol (mean infusion rates of 1.62–2.8 mg/kg/h) with midazolam (mean infusion rates of 0.04–0.2 mg/kg/h) for varying periods, the proportion of time that patients were adequately sedated was similar with both agents (table IV).[8,9,12,37,110] The quality of sedation was based on an assessment made by nursing staff using the Ramsay sedation scale, the Glasgow coma scale and/or a modified version of either. Sedation was generally considered effective if the score was within a predetermined range on the sedation scale. Continuous infusions of propofol achieved adequate levels of sedation 62–97% of the time compared with 57–93% of the time with midazolam (table IV).[8,9,12,37,110] In one study of 88 patients who were sedated for periods of <24 hours to >7 days, the time spent with adequate sedation significantly favoured propofol (93%) compared with midazolam (82%) [p < 0.05].[41] Propofol also achieved adequate sedation levels for similar periods to lorazepam or midazolam,[110] dexmedetomidine[57] or isoflurane (table IV).[111]
One nonblind study evaluated the quality of sedation by using a nurses’s rating, which assessed the patient’s response to endotracheal tube suctioning or manipulation, turning or repositioning, and dressing changes.[25] In postoperative, intubated, general surgical or orthopaedic patients requiring sedation for 12–24 hours, patients receiving propofol (n = 30) achieved a significantly better level of sedation than those receiving midazolam (n = 30) [p < 0.05] (results not presented in table IV).[25]
4.1.2 Rate of Recovery
The pharmacokinetic profile of propofol allows for a rapid rate of recovery from sedation due to rapid redistribution and metabolic clearance (section 3). Clinical trials have demonstrated that the rate of recovery following cessation of the sedative infusion is faster with propofol than midazolam following short- (≤24 hours), medium- (24–72 hours) and long-term (>72 hours) sedation (table IV).[8–15,41,64]
In the one study comparing sedation with propofol (n = 10) or dexmedetomidine (n = 10), rates of recovery were rapid in both treatment groups; respective mean times to extubation were 28 and 29 minutes (table IV).[57]
Short- (≤24 Hours) and Medium-Term (24–72 Hours) Sedation
Most studies in patients receiving sedation for up to 72 hours demonstrated a significantly shorter recovery time with propofol than with midazolam (table IV).[8,10,11,41,64] For example, in a subgroup analysis assessing the time to weaning from the ventilator after approximately 20 hours of sedation; the mean time to successful independent breathing was 5 minutes for propofol recipients (n = 21) compared with 148 minutes for midazolam recipients (n = 18) [p < 0.001] (table IV).[8]
Short-term changes in the depth of sedation are often required in the ICU to facilitate procedures such as physiotherapy or changing the patient’s position. Propofol (n = 10) provided better control of the depth of sedation than midazolam (n = 9) when infusions were altered to facilitate short periods of physiotherapy in patients requiring mechanical ventilation following a surgical repair of an abdominal aortic aneurysm.[11] After 24 hours of mechanical ventilation, the infusion rate of the sedative was increased to deepen the level of sedation from 3 on the Ramsay sedation scale to 5, and a standard regimen of physiotherapy was given for 12–16 minutes. During physiotherapy, patients treated with propofol achieved the desired sedation level more often than those treated with midazolam (53.9% vs 25.7% of the time; p < 0.01). After physiotherapy, infusion rates were again adjusted to resume a Ramsay sedation level of 3. Patients receiving propofol reawakened to level 3 faster than those receiving midazolam (8.3 vs 92.8 minutes; p < 0.05). During physiotherapy, a similar number of dosage adjustments were required with both agents to achieve the desired sedation level, whereas after physiotherapy, fewer dosage adjustments were needed to the propofol infusion than to the midazolam infusion (0.4 vs 1.8, respectively; p < 0.05).[11]
Propofol (n = 37) also produced faster, more reliable wake-up times than midazolam (n = 36) in a further subgroup comparison of patients who were not awake at time zero in a randomised, nonblind study (not tabulated).[27] Recovery from sedation in <60 minutes was compared in the propofol and midazolam treatment groups by the ability to perform four tasks: open eyes on verbal command (p = 0.007); follow the observer with eyes (p = 0.01); hand grasp on command (p = 0.017); and stick out tongue on command (not significant).[27]
Long-Term (>72 hours) Sedation
In patients sedated for >72 hours, the improvement in time to recovery and extubation with propofol compared with midazolam was generally more marked than the time differences to recovery and extubation observed between the two agents after shorter duration infusions (table IV).[9,12,14,41,64]
In all studies of patients receiving long-term sedation (ranging from approximately 80 hours to 13 days), recovery times and the time to extubation were significantly shorter with propofol treatment than with midazolam treatment (table IV).[9,12,14,41,64] Furthermore, a subgroup analysis in one of these trials indicated that even in patients deeply sedated at the time the infusion was stopped, the time to recovery was rapid, and more rapid with propofol (n = 19) than with midazolam (n = 9) [27 vs 237 minutes, p < 0.01].[12] Recovery time was defined as the time taken to achieve the maximum score on a sedation scale based on the Glasgow coma scale.[12]
Noncomparative studies further support these data, showing that after ICU sedation of periods of up to 7 days, the time to recovery associated with propofol was rapid.[40,114,115]
Comparisons of Short-, Medium- and Long-Term Sedation
A greater predictability in recovery time with propofol than with midazolam was demonstrated by the correlation of the duration of propofol administration with recovery times.[41] Infusions of propofol for <24 hours (n = 20), from 24 hours to 7 days (n = 16) and >7 days (n = 10) demonstrated correlations with the time to extubation (r = 0.83, 0.94 and 0.90, respectively) and with the time to recovery (r = 0.98, 0.88 and 0.92, respectively), whereas no correlation was observed in the midazolam group.[41]
Recovery times after short- (<24 hours), medium- (≥24 and <72 hours) or long-term (≥72 hours) sedation with propofol or midazolam were compared in 99 critically ill patients in four ICUs in Canada.[64] The use of propofol allowed for a significantly shorter time to tracheal extubation than did midazolam in the short- and long-term sedation subgroups (p < 0.05) [figure 3].[64] Of interest in this study is the observation that, despite earlier extubation with propofol than with midazolam, the time to ICU discharge was longer with propofol in the short- and medium-term sedation subgroups. The reason for this finding is unclear.[64]
Time from withdrawal of sedation with propofol or midazolam to tracheal extubation and intensive care unit (ICU) discharge. Critically ill patients requiring continuous sedation following general or cardiac surgery or for the management of medical conditions were randomised to receive infusions of either propofol or midazolam in a multicentre, nonblind trial. Following initial doses of propofol 0.3–0.6 mg/kg/h or midazolam 0.012–0.024 mg/kg/h, dosages were titrated to achieve a target Ramsay sedation score specified for each patient. Analysis was intent-to-treat. Patients were also stratified according to their predicted sedation time based on their predicted need for mechanical ventilation: short term <24h (n = 47); medium term ≥24h but <72h (n = 38); and long term ≥72h (n = 14).[64] *p < 0.05 vs midazolam.
4.2 Sedation Following Cardiac Surgery
After surgery involving cardiopulmonary bypass, a short period of controlled mechanical ventilation is often necessary as patients are vulnerable to myocardial ischaemia and may be haemodynamically unstable and hypothermic.[17] Intravenous sedation and analgesia can aid intubation by controlling patient agitation as well as controlling any associated hypertension and tachycardia.[24]
The efficacy of propofol has been evaluated following CABG surgery in several comparative, randomised clinical trials, which are summarised in table V. Most trials compared propofol with midazolam. Patients were aged over 16 years and were considered to have a probable need for mechanical ventilation for a short period (approximately 8–16 hours) postoperatively. Exclusion criteria included left ventricular dysfunction (ejection fraction <35–45%)[17,19,24,56] or perioperative haemodynamic instability.[18] In most studies, patients were also excluded if they had a history of hepatic, renal, CNS or metabolic dysfunction.[17–19,24]
Propofol maintained patients at the desired level of sedation for a similar[16,18,19,24,56] or greater[20,116] percentage of the sedation period to that achieved by midazolam (60–93% vs 48–88%) [table V]. Compared with alfentanil[117] or oxycodone plus thiopental,[118] propofol maintained adequate sedation for a similar period (table V).
The mean time to spontaneous ventilation was significantly shorter (p < 0.05 for all comparisons) in patients treated with propofol than in those receiving midazolam in all studies assessing this endpoint (table V).[16–18] Compared with alfentanil, propofol was associated with a similar time to spontaneous ventilation.[117] In most studies, propofol recipients were extubated significantly earlier than midazolam recipients (p < 0.05).[16,17,19,20] In one study, there was a trend toward a shorter time to extubation with propofol (p < 0.059)[18] and in two studies,[56,116] the time to extubation was similar with both propofol and midazolam (table V).
In the first 12 hours following a cardiopulmonary bypass procedure, haemodynamic episodes often occur. Sedative agents have the potential to affect haemodynamic response, and their action on cardiovascular parameters (section 2.2) are an important consideration during this postoperative period.[119]
Compared with midazolam, propofol was associated with a similar cardiovascular outcome during the first 12 hours following CABG surgery in a randomised, double-blind study.[119] Patients who were haemodynamically stable after surgery received propofol (n = 117) or midazolam (n = 150) for a minimum of 12 hours after aortic unclamping. Dosages of both agents were titrated to achieve sedation level 5 on a modified Ramsay scale, and were supplemented as necessary with bolus doses of morphine. The incidence of myocardial ischaemia was not different between the two treatment groups (12% with propofol vs 13% with midazolam), and at least one haemodynamic episode occurred in 93% of patients in both groups (specific events are illustrated in figure 4 and discussed in section 5.1).[119] Results of other studies also demonstrated similar cardiac outcomes with propofol or midazolam (section 2).[16,18,20,56,116]
Incidence of haemodynamic events occurring during postoperative sedation after coronary artery bypass graft surgery in a randomised, double-blind trial.[119] Patients who were haemodynamically stable after surgery received propofol (n = 117) or midazolam (n = 150) for a minimum of 12 hours after aortic unclamping. Events were recorded postoperatively during the first hour, hours 1–6 and hours 6–12. Dosages of both agents were titrated to achieve sedation level 5 on a modified Ramsay scale and were supplemented as necessary with bolus doses of morphine.[119] * p < 0.01 vs midazolam.
The requirement for concomitant vasodilators (sodium nitroprusside or nitroglycerin) to treat postoperative hypertension was similar or reduced with propofol sedation compared with midazolam.[16–19,24,56]
4.3 Sedation Following Head Injury or Neurosurgery
In patients with severe head trauma, sedation is required to control raised intracranial pressure (while maintaining cerebral perfusion pressure >60–70mm Hg) and to facilitate mechanical ventilation.[32] Also of primary importance in this patient group is the need for rapid reversibility of sedation to enable frequent assessment of the neurological condition.[120]
In noncomparative studies in patients with head injury, propofol has been shown to maintain mean cerebral perfusion pressure >60mm Hg and reduce or maintain mean intracranial pressure.[32,34]
In comparative studies, the effect of propofol on intracranial pressure in patients following head injury was similar to that of fentanyl[35] or pentobarbital plus morphine[121] and appeared more effective than midazolam plus morphine[33] or morphine alone.[122] For example, in comatose patients with severe head injury, intracranial pressure was unchanged in recipients of a 24-hour infusion of propofol (1–3 mg/kg/h) or fentanyl (0.3–0.5 mg/h), both in combination with pancuronium (results reported in an abstract).[35] However, in a subgroup analysis of this study, patients with high intracranial pressure (>16mm Hg) treated with propofol had a greater decrease in intracranial pressure (from 20 to 8mm Hg) than those treated with fentanyl (from 20 to 13mm Hg) [p < 0.05]. Cranial perfusion pressure remained above 70mm Hg in both high and low intracranial pressure (≤16mm Hg) subgroups.[35]
In a randomised, double-blind trial of patients with moderate or severe head injuries, intracranial pressure and cerebral perfusion pressure were generally similar in groups treated with 2% propofol (n = 23) or morphine (n = 19), but on day 3 intracranial pressure was lower in patients treated with propofol than with morphine (14mm Hg vs 18mm Hg; p < 0.05).[122] The mean infusion rate and duration of therapy was 3.3 mg/kg/h and 95 hours for the propofol group, and 1.3 mg/h and 70 hours in the morphine group. Prognostic indicators in the propofol group were generally worse than those in the morphine group, with a higher percentage of patients receiving propofol recording a Glasgow Coma Scale score of 3–5 (p < 0.05).[122] Patients receiving propofol required fewer neuromuscular blocking agents, benzodiazepines and pentobarbital than those receiving morphine. The 6-month outcome, as assessed by the Glasgow Outcome Scale, was similar in both treatment groups.[122]
In a further small comparative study of patients with severe head injury, propofol (mean infusion 3.6 mg/kg/h, mean duration 22.5 hours) produced adequate control of intracranial pressure in all patients (n = 10), whereas adequate control was achieved in only three of seven patients receiving morphine plus midazolam (mean dose 47.1mg, mean duration 20 hours) [levels of significance were not reported]. [33]
Following neurosurgery, sedation is required to facilitate mechanical ventilation and minimise physiological stress, which may compromise cerebral function.[123] As in the treatment of head injury, rapid reversal of sedation following neurosurgery is preferable, thus enabling assessment of the patient’s neurological condition. Noncomparative trials in such patients found that propofol provided adequate sedation with haemodynamic stability[124] and allowed rapid recovery.[125]
In comparison with midazolam (0.075 mg/kg/h), propofol (2.67 mg/kg/h) produced similar effects on cardiovascular and intracranial pressure measurements in patients (n = 20) following neurosurgery.[126] Both treatment groups were judged to have experienced a similar quality of sedation, but patients receiving propofol were discharged earlier from the ICU (6.25 vs 9.79 hours).[126]
Propofol (n = 12) was associated with a more rapid rate of recovery than methohexital (n = 12) following sedation of neurosurgical patients, as observed in a retrospective study reported in an abstract.[127] Within 6 hours of cessation of the infusion, 75% of propofol recipients had completely recovered compared with 58% of methohexital recipients (no levels of significance were given).
4.4 Sedation in Special Patient Populations
Chronic obstructive pulmonary disease (COPD) can lead to acute respiratory failure and a requirement for mechanical ventilation in some patients. In a comparative trial of patients with COPD who required artificial ventilation, propofol (n = 5) was associated with a superior overall quality of sedation, as assessed by nursing staff, than midazolam (n = 6) [p = 0.0173].[67]
Several case studies report that propofol has been used successfully in the ICU to sedate patients with status epilepticus unresponsive to conventional therapy.[128–133] A retrospective study of 14 patients with nonconvulsive status epilepticus (NCSE), reported in an abstract, found that treatment with intravenous propofol effectively controlled NCSE in many but not all patients; the underlying cause of the condition was the most important prognostic factor.[134]
Propofol infusions have also been used successfully in patients with delirium tremens[135–137] and tetanus.[138–140] Continuous infusions of propofol in patients with tetanus, some for as long as 25 days, have provided a good level of sedation and a rapid rate of recovery, with patients becoming fully awake at 30 minutes to a few hours after discontinuation of the infusion.[138–140]
5. Tolerability
This section discusses the tolerability profile of propofol when used for ICU sedation in patients aged >16 years, using data from clinical trials discussed in section 4, as well as information from the manufacturer. Some data from studies in patients receiving propofol anaesthesia have also been included. Because patients requiring sedation in an ICU are generally critically ill, it is often difficult to determine whether an adverse event is related to propofol therapy, the underlying disease or other medications. According to the manufacturer’s prescribing information, most reported adverse events associated with propofol are mild and transitory.[3]
5.1 Cardiovascular Events
The cardiovascular depressant effects associated with propofol, described in section 2.2, most commonly manifest as hypotension and to a lesser extent as a reduced heart rate. In clinical trials discussed in section 4, hypotensive effects were observed with all sedative agents but rarely led to interruption of the infusion. Haemodynamic parameters were maintained within prescribed limits by the administration of inotropic drugs and intravenous fluids as clinically indicated. Thus, significant differences in haemodynamic parameters were generally not observed between treatment groups.[8,12,116,126] However, if an initial bolus dose of sedative was given at the onset of sedation, transient hypotension was associated with propofol[10] and was greater than that observed with the initial bolus dose of midazolam.[14,18,24,25] According to the manufacturer’s prescribing information, hypotension occurs in 26% of patients receiving propofol sedation in the ICU.[3]
The incidence of haemodynamic events (93%) was similar with both propofol (n = 117) and midazolam (n = 150) in patients following CABG surgery in a randomised, double-blind study, but the nature of events differed.[119] Compared with midazolam, propofol was associated with less tachycardia and hypertension but more hypotension from 1 to 12 hours from the start of sedation. Respective limits for tachycardia, hypertension and hypotension for the postoperative period were 100 beats/min, 140mm Hg and 90mm Hg. Results are summarised in figure 4. The incidence of hypotension between hours 1 and 6 was 49% in patients treated with propofol and 34% in those treated with midazolam (p < 0.01) [figure 4].[119]
Because of the hypotension associated with propofol, particular care should be taken with the administration of the drug to the elderly and to patients who are hypotensive (see section 7), hypovolaemic or haemodynamically unstable.
Although a causal relationship has not been confirmed, arrhythmia, atrial fibrillation, bigeminy, cardiac arrest, extrasystole, right heart failure and ventricular tachycardia have been observed in <1% of patients receiving propofol sedation in the ICU.[3]
5.1.1 Propofol-Infusion Syndrome
In the early 1990s, several case reports suggested an association between sedation with high-dose propofol (>4 mg/kg/h) and myocardial failure and death in children with respiratory tract infections.[141] A possible propofol-infusion syndrome was identified and defined as follows: a relatively sudden onset of marked bradycardia resistant to treatment, with progression to asystole; the presence of lipaemia; a clinically enlarged liver secondary to fatty infiltration; the presence of severe metabolic acidosis; and the presence of muscle involvement with evidence of rhabdomyolysis or myoglobinuria.[142] A direct causal link with propofol has not been established, but the syndrome appears to be related to propofol to some degree.[143] Although the syndrome has only been associated with high-dose infusions,[143] propofol is not recommended for sedation in children as efficacy and tolerability have not been demonstrated.[101]
More recently, case reports have suggested a similar propofol-infusion syndrome in critically ill adults.[144,145] In a retrospective cohort analysis of critically ill adults with head injuries receiving long-term (>58 hours), high-dose (>5 mg/kg/h) infusions for the control of ICP, 7 of 67 patients developed an apparent propofol-infusion syndrome; 2% propofol was used in five of these seven cases.[144]
5.2 Neurological Events
Although propofol has demonstrated anticonvulsant properties,[1] neuroexcitatory events, manifesting as abnormal movements, have been associated with its use as an anaesthetic agent.[146–149] It is not clear whether these abnormal movements are the result of true seizure activity or due to a noncortical event.[146]
In the clinical trials of patients receiving propofol sedation in the ICU discussed in section 4, there were no reports of neurological effects attributable to propofol. In a crossover trial comparing propofol and isoflurane,[111] three patients reported visual hallucinations during and/or after the cessation of sedation. All patients received propofol initially followed by isoflurane.
Agitation has occurred in <1% of patients receiving propofol sedation in the ICU.[3]
5.3 Infection
Because propofol is formulated as a lipid emulsion, it provides an excellent medium for the growth of a variety of organisms. In response to reports of infection associated with propofol anaesthesia, which in most cases appeared to be related to extrinsic microbial contamination due to a lapse in aseptic technique, in 1996 an additional formulation of propofol containing the bacteriostatic agent EDTA also became available (section 2.8).[2] Since its introduction, the incidence of fever and infections (approximately 20 per year) has been virtually eliminated.[2,150]
In an observational study of 100 patients receiving a total of 302 propofol infusions (without EDTA) for sedation in the ICU for approximately 4–6 hours, there were no episodes of infection or colonisation of the infusion that could be attributed to contaminated drug.[151]
Similarly, the results of a study assessing the extrinsic contamination of propofol infusions in the ICU suggest that the risk of bacterial and fungal contamination is low if standard infection control practices are adhered to (section 7). Data from this study also indicate that longer periods of infusion (>24 hours) may be associated with a higher risk of contamination.[152] However, the manufacturer’s prescribing information, in accordance with guidelines for other lipid emulsions, clearly states that a single infusion of propofol must not exceed 12 hours (section 7).[101] Both the reservoir of propofol and the infusion line must be replaced at 12 hours or at the end of a procedure, whichever is the sooner.[101]
In the clinical trials discussed in section 4, there were no reports of infection related to propofol infusions. The risk of nosocomial infection, therefore, appears low during the routine use of propofol for sedation in the ICU. However, aseptic techniques must be followed during handling and preparation (section 7), irrespective of whether the clinician is using original propofol or a formulation containing EDTA.[101]
5.4 Other Events
One of the most commonly reported adverse events associated with propofol is pain on injection. However, this is not usually a problem in the ICU as the preferred route of administration is via a central line.[153] Local pain on injection can be minimised by using larger veins in the forearm or antecubital fossa.[101]
The lipid content of the propofol infusion increases serum triglyceride concentrations when given long term (>3 days) [section 2.5]. In some studies, concentrations returned to normal when the infusion was stopped,[9,41] but in another trial, return to presedation levels was variable and in some instances took several days (section 2.5).[40] A rise in triglyceride concentrations was observed in all ten patients sedated with propofol for >7 days,[41] and in 11 of 54 patients sedated with propofol for an average of ≊140 hours (mean serum triglyceride concentration 6.6 mmol/L).[9] In both trials, mean serum triglyceride concentrations returned to within normal limits (3.7 mmol/L)[9] in all patients after stopping the infusion[41] or within 72 hours.[9] Patients receiving sedation with propofol for >3 days should have their lipid profiles closely monitored. In addition, the calorific value of concomitant parenteral nutrition should be reduced to compensate for the lipid contained in the propofol infusion (section 7).[3] The use of 2% propofol halves the lipid load administered to critically ill patients and has been associated with less hypertriglyceridaemia than 1% propofol (section 2.5).[42]
Respiratory acidosis has been reported during weaning from the ventilator in approximately 3–10% of patients receiving propofol sedation in the ICU.[3] The excretion of the phenolic metabolites of propofol has led to green discolouration of the urine in isolated cases, particularly after long-term infusions.[154,155] This phenomenon of green discolouration has also been seen in the liver[156] and hair.[157] The effect is transient and does not appear to affect renal function or be of clinical significance. On rare occasions, anaphylactoid reactions have been associated with propofol administration[158,159] and, following high dosages (4 mg/kg/h), there have been rare reports of rhabdomyolysis.[101]
6. Pharmacoeconomic Considerations
Cost considerations are important in evaluating the appropriate sedative for critically ill patients during mechanical ventilation in the ICU. Two of the most commonly used ICU sedatives are propofol and midazolam, and both agents have been compared from a clinical (section 4) and economic viewpoint. Propofol has a higher acquisition cost than midazolam, but clinical studies indicate a faster recovery time (sections 4.1.2 and 4.2). Whether this faster recovery and subsequent improved time to extubation can offset the increased drug cost has been evaluated in several pharmacoeconomic studies (table VI).[9,41,160–163]
Except for three cost-benefit analyses,[41,43,163] all studies were cost analyses and performed from a healthcare perspective only. Inclusion and exclusion criteria were similar to those of clinical studies discussed in section 4, but patients with head injuries[9,161,163] or in a coma caused by a cerebrovascular accident or of unknown cause[160] were also excluded. Periods of sedation varied, and dosages were titrated to achieve a target level of sedation.
In all studies evaluated, sedation with propofol led to a faster time to extubation than sedation with midazolam,[9,41,160–164] and in all studies except one[160] this led to a lower total ICU cost associated with propofol, albeit only in the short term in two studies.[41,163]
The relationship between early tracheal extubation and reduced ICU costs compared with late extubation was demonstrated in 100 patients after CABG surgery.[164] Early tracheal extubation reduced actual total ICU costs per patient by 18% compared with late extubation ($Can4830 vs $Can5892, respectively; p < 0.009), with most of the savings made in the area of nursing and supplies (actual year of costing not reported). Results are illustrated in figure 5. Compared with late extubation, early extubation led to a reduced length of stay in the ICU and in the hospital without increasing the incidence or costs of complications.[164]
Mean actual cost per patient during an intensive care unit (ICU) stay after coronary artery bypass graft surgery. Patients were randomised to early extubation (1–6 hours after the start of sedation) or late extubation (12–22 hours after the start of sedation) in a nonblind study.[164] Patients in the early-extubation group (n = 41) received an infusion of propofol 2–6 mg/kg/h at the start of anaesthesia, which was continued for 1–4 hours in the ICU. Patients in the late extubation group (n = 41) received anaesthesia with fentanyl, isoflurane and midazolam, followed by routine morphine and midazolam (1–3 mg/h) in the ICU. Year of actual costing was not reported. RT = respiratory therapy; * p < 0.05, ** p ≤ 0.009 vs comparator.
6.1 Short- and Medium-Term Sedation
The combination sedative regimen of propofol plus alfentanil had a better pharmacoeconomic profile than midazolam plus morphine because, as shown in other studies, times to extubation and ICU discharge were shorter.[161] The mean period of sedation was not reported, but the study included patients requiring mechanical ventilation for at least 12 hours (one patient was sedated for 7 days with morphine and midazolam). A cost analysis of both sedation regimens assessed costs of drug acquisition and administration, as well as nondrug-related costs based on an ICU cost per patient per day. Costs were given in pounds sterling; at the time of the study £1 was equivalent to $US1.59. The median time to extubation was 3 hours for the propofol group (n = 17) and 50 hours for the midazolam group (n = 9) [p = 0.006]. Respective times until patients were fit for transfer from the ICU were 6 and 57 hours (p = 0.0012). The drug-related costs for propofol and alfentanil were higher than those for morphine and midazolam (p = 0.0054), but the nondrug-related costs, which included additional costs incurred from a longer stay in the ICU, were higher for patients receiving midazolam and morphine (p = 0.0009). The total cost per patient for a stay in ICU was about two-thirds less for patients treated with propofol plus alfentanil compared with patients treated with midazolam plus morphine (£3095 vs £9511; p = 0.0013) [table VI).[161]
The combination of propofol and low-dose fentanyl had a lower, albeit nonsignificant, total cost per patient than midazolam and high-dose fentanyl in a trial in patients receiving sedation for up to 48 hours after undergoing elective cardiac surgery (table VI).[162] The study aimed to compare drug costs and nursing dependency of patients and was not powered for economic outcomes. Drug costs were obtained from the British National Formulary (September 1993). Nursing costs were calculated by converting patient extubation and discharge times into shifts required, based on one nurse for each ventilated patient and one nurse to two extubated patients. Patients receiving propofol and fentanyl (n = 37) had a shorter median time to extubation from ICU entry than patients receiving midazolam and fentanyl (n = 33) [4.33 vs 9.17 hours]. Median time to discharge from the ICU was similar (22.42 vs 23.57 hours, respectively), but an ICU discharge policy only allowed unit discharges between 0830 and 1900 hours. Mean nursing shifts required for patients in the propofol group were 2.95 versus 3.68 in the midazolam group. The total cost per patient, determined by adding nursing costs to total drug costs, was £315.52 in the propofol group compared with £358.75 in the midazolam group (not significant) [table VI]. However, a further analysis of log-transformed data demonstrated that, on average, the total cost in the propofol group was 13.3% lower than that in the midazolam group (p = 0.043).[162]
In contrast to the results above, a recent Canadian, nonblind, multicentre study demonstrated similar total ICU costs with propofol or midazolam (approximate duration of infusion was 16 hours) [table VI].[160] Treatment costs were recorded for each patient during his/her stay in the ICU, including physician visits, nursing time, other health professional contacts, diagnostic tests and medications. Sedative costs were calculated from the recorded drug quantity, including wastage, and the respective drug prices: $Can43.01 for 1000mg/100mL of propofol and $Can20.21 for 50mg/10mL of midazolam. Fixed ICU costs included overheads and opportunity cost of resources, as well as 5% global depreciation of capital equipment. All costs were expressed in 1997 Canadian dollars. For analytical convenience, the length of stay in the ICU was divided into three consecutive periods: from admission to the start of sedation, from the beginning of sedation to termination of sedation and extubation, and from extubation to discharge from the ICU. Although the difference in time spent at each period did not reach statistical significance between treatment groups, further analysis of segments within each period showed that the time from sedation to ‘ready for extubation’ was significantly shorter in the propofol group (n = 46) than in the midazolam group (n = 53) [2.5 vs 7.1 hours; p = 0.001].[160]
The total median costs for the ICU stay were $Can5718 for each patient treated with propofol and $Can5950 for each patient treated with midazolam (table VI), and the total median sedative costs per patient were $Can86.02 and $Can40.42, respectively.[160] Neither difference was significant. As a result, the total costs per patient did not differ between treatment groups ($Can5765 in the propofol group vs $Can5998 in the midazolam group). A sensitivity analysis suggested that the incremental cost per patient for propofol varied from savings of $Can2709 to an extra cost of $Can114.[160]
A further sensitivity analysis of this study[160] was based on a hypothetical model that evaluated potential cost savings through improved discharge planning with propofol, because of the shorter time from sedation to ‘ready for extubation’ compared with midazolam. Log-transformed sedation to extubation time and sedative drug cost were modelled as dependent variables adjusted by the duration of sedation. In this analysis, time to extubation with propofol appeared to be 4.2-times faster and drug costs 3.6-times higher than midazolam. Based on this model, the sensitivity analysis demonstrated a potential saving with propofol of between $Can244 and $Can570 for each patient when ICU daily cost and reduced extubation times were varied within a range of ±30%. Unlike other studies,[9,41,163] this model also suggested that as the duration of sedation increased, the potential savings associated with propofol increased.[160]
6.2 Long-Term Sedation
In a Spanish study published in 1997, a more favourable economic profile was demonstrated with propofol than with midazolam because of a faster time from discontinuation of sedation to extubation (34.8 vs 97.9 hours; p < 0.0001).[9] Dosages ranged from 1 to 6 mg/kg/h for propofol and 0.1 to 0.5 mg/kg/h for midazolam, and the mean sedation period was ≊ 5.5 days. The total actual cost per patient, including drug costs ($US0.026/mg for propofol and $US0.123/mg for midazolam) and costs during sedation and weaning periods, was $US9466 for propofol (n = 54) and $US10 828 for midazolam (n = 54), a cost difference of $US1362 (table VI).[9]
A cost predictive model was developed based on the results of this study.[9] Average costs for mechanical sedation in the ICU were set at $US54/hour, and weaning costs took into account the cost of therapeutic failure, which included 11 patients with hypertriglyceridaemia in the propofol group, and death. An assessment of weaning times associated with each agent revealed that with propofol, weaning time increased if the duration of sedation was prolonged. Based on this model, the study found that the cost difference between propofol and midazolam reduces and eventually disappears as the duration of sedation becomes longer, assuming other factors do not vary.[9]
This cost predictive model, together with historical data from the same trial, was used in a more recent pharmacoeconomic study comparing 1% and 2% propofol.[43] When more prolonged sedation is indicated, 2% propofol provides the advantage of less lipid administration and, therefore, less hypertriglyceridaemia (sections 2.5 and 5.4). The frequency of hypertriglyceridaemia with 1% propofol (n = 54) was 20.4% compared with 3.9% with 2% propofol (n = 51), and the therapeutic failure rates were 33.4% and 19.6%, respectively (not significant). The study aimed to determine if this improved therapeutic failure rate with 2% propofol could lead to a cost advantage over 1% propofol. The weaning time between patients treated with 1% or 2% propofol was similar, and the difference in weaning time was similar between midazolam and 1% or 2% propofol. However, an additional cost benefit over that shown between 1% propofol and midazolam was not demonstrated, as a higher dosage of 2% propofol than 1% propofol was required in the first 48 hours of sedation (p < 0.05).[43]
6.3 Comparisons of Short-, Medium- and Long-Term Sedation
Two trials compared cost differences between groups of patients receiving propofol or midazolam for short-, medium- or long-term sedation.[41,163] In both trials, a cost advantage was observed for propofol compared with midazolam in patients receiving short-term sedation (<24 hours[41] or up to 72 hours[163] ) but not in those receiving longer-term sedation (table VI).[41,163]
In one of these studies (n = 88),[41] the acquisition cost of propofol was three-times higher than that of midazolam in the short-term sedation subgroup (<24 hours; n = 40), but the longer stay in the ICU associated with midazolam lead to a postsedation cost four-times higher than that of propofol and a significantly higher total sedation cost per patient (Pta10 900 vs Pta8900; p < 0.05) [table VI]. In all subgroups, the time to extubation and total recovery (time at which the patient could be discharged to a conventional ward or intermediate care unit) were significantly shorter with propofol than with midazolam (p < 0.05). However, this did not result in a significant cost advantage for the propofol recipients in the medium- (24 hours to 7 days) or long-term (>7 days) sedation subgroups.[41]
A further Spanish cost analysis also demonstrated a lower total cost of sedation with propofol (n = 53) than with midazolam (n = 51) or morphine plus diazepam (n = 35) in patients requiring short-term sedation (up to 72 hours) [Pta9000, Pta10 900 and Pta12 400, respectively; table VI].[163] Total costs were similar with both propofol or midazolam in the medium- (3–5 days) or long-term (>5 days) sedation groups. Statistical analyses were not performed. The total cost included the cost of drugs, the cost of the ICU stay (determined on a price-per-hour basis) and the cost of any additional care required before transfer to a ward.[163]
7. Dosage and Administration
To provide intensive care sedation in mechanically ventilated patients, propofol should be administered by continuous infusion. The initial rate should be slow, to minimise hypotension, and titrated to achieve the desired clinical effect.[3] The recommended initial rate of infusion is 0.3 mg/kg/h, increasing in increments of 0.3–0.6 mg/kg/h at intervals of at least 5 minutes, as clinically indicated.[3] A rate of between 0.3 and 3.0 mg/kg/h should achieve satisfactory sedation.[3] Bolus doses of 1% propofol may be given if clinically indicated and if hypotension is not likely to occur, but bolus injection of 2% propofol is not recommended.[3] Patients who have received large dosages of opioid analgesics or narcotics should receive reduced dosages of propofol.[3] Elderly patients (aged >55 years) also require a reduced propofol infusion rate (1.8 mg/kg/h) [section 3.3].[3]
Dosage requirements are variable between patients and may change over time. Titration to clinical response with daily assessment of sedation levels and CNS function are important to determine the minimum dosage required.[3] A higher than necessary dosage will lead to high plasma concentrations of propofol, which can result in a longer time to recovery (section 3.2). A light level of sedation is recommended throughout the weaning process, with discontinuation of the infusion 10–15 minutes before extubation.[3]
The oil-in-water propofol emulsion supports the growth of micro-organisms (section 5.3). Strict aseptic technique must be used during the handling and preparation of the product, both with the original formulation and that containing the bacteriostatic agent EDTA. In accordance with guidelines for other lipid emulsions, a single infusion of propofol must not exceed 12 hours.[101] When a procedure is completed or at 12 hours, whichever is sooner, both the reservoir of propofol and the infusion line must be discarded and replaced.[101]
The 1% formulation of propofol may be used undiluted or diluted with 5% dextrose only, and dilutions should not exceed one in five.[101] 2% propofol should not be diluted. Once the drug is prepared for use, administration should commence within 6 hours. It is recommended that the drug be administered via syringe pumps or volumetric pumps to control infusion rates.[3]
Elevations in serum triglyceride concentrations may occur with prolonged infusions (>3 days) of propofol (section 2.5), and concentrations should be monitored in patients at risk. The quantity of concomitant enteral or parenteral nutrition should be reduced to compensate for the lipid content of the propofol infusion (1mL = 0.1g of fat [1.1 kcal]).[3]
Because of the risk of cardiac arrest associated with high doses of propofol (section 5.1), patients should be monitored for unexplained metabolic acidosis or arrhythmias.[165] Caution should be used in patients receiving long-term (>48 hours), high-dose (>5 mg/kg/h) propofol infusions.[166]
During administration of the propofol formulation containing EDTA, the need for supplemental zinc should be considered (section 2.8).[101] Renal function was not significantly affected in patients with renal impairment sedated with propofol containing EDTA (section 3.3.3).
8. Place of Propofol in the Intensive Care Sedation of Adults
Effective sedation and analgesia are essential in the care of the critically ill to provide patient comfort and avoid the risks associated with anxiety and agitation. Stress-induced response to the ICU environment, the presence of an endotracheal tube, sleep deprivation and pain can lead to comorbid haemodynamic and metabolic consequences, such as hypertension, tachycardia, increased oxygen consumption, reduced immune function, and in some cases, delirium.[167]
The ideal level of sedation differs for each patient and may change throughout the course of care depending on his/her condition and response to therapy.[168] However, the primary aim for most patients is to maintain a sleepy but easily aroused state. Deeper levels of sedation are indicated in some patients, such as those receiving neuromuscular blockade.[168] To ensure that the changing needs of the patient are met, the depth and quality of sedation should be monitored. This is most commonly achieved by the use of one or more of several sedation scales (e.g. Ramsay Sedation Scale, Riker Sedation-Agitation Scale [SAS] and Motor Activity Assessment Scale [MAAS]).[165]
Sedative agents induce anxiolysis, hypnosis and often a degree of amnesia, but most do not have analgesic activity.[168] The most frequently used sedatives in the ICU are the benzodiazepines (e.g. midazolam and lorazepam) or propofol, and both are usually given in combination with opioid analgesics (e.g. morphine), which can also have sedative effects.[73] The benzodiazepines provide effective sedation and also have anxiolytic, anticonvulsant and amnesic effects.[169] Prolonged administration (>24 hours) can result in drug accumulation leading to delayed recovery, and withdrawal symptoms have been observed when the infusion was stopped abruptly.[170] The benzodiazepines have also been associated with dose-related respiratory depression and hypotension.[170] Compared with midazolam, lorazepam has a slower onset of action but a lower cost and, therefore, is an option for long-term sedation.[171]
Propofol provides effective sedation, and plasma concentrations correlate with the depth of sedation (section 2.1). The drug also provides anxiolytic and anticonvulsant effects (section 4.4) but does not induce the same level of amnesia as the benzodiazepines (section 2.4.3). Because propofol is highly lipophilic, it rapidly crosses the blood-brain barrier to produce a rapid onset of action. This fast onset of sedation, together with a short duration of action leading to rapid recovery (section 3.1 and 3.2), are the main advantages of propofol over other sedative agents. Even when propofol is administered for prolonged periods (>7 days), recovery from sedation is rapid (section 4.1.2 and 4.2). However, over time the volume of distribution increases and is greater with long-term therapy (up to several days) than short-term infusions (<24 hours) [section 3.1]. This reflects the increased peripheral distribution that occurs over time but is usually of little clinical relevance, as rapid clearance results in subtherapeutic plasma concentrations once the infusion is stopped. Titration of the dosage to achieve the desired clinical effect is recommended (section 7) to ensure that minimal dosages are given and to avoid the risk of excess drug accumulation in the long term, which could result in a delayed time to recovery. Although long-term sedation has not been studied in patients with renal or hepatic impairment, propofol metabolism does not appear to be affected in these patients (section 3.3.3).
Propofol generally provides good haemodynamic stability and some beneficial cardiovascular effects (section 2.2). Moreover, systemic vascular resistance and heart rate are reduced (section 2.2.1), which can be beneficial in patients at risk for a stress-induced sympathetic response. In addition, total VO2 appears to be reduced with higher dosages of propofol (2 mg/kg/h) [section 2.2.2], thereby diminishing cardiac workload, a favourable effect in patients after cardiac surgery. However, transient marked hypotension is associated with bolus administration (section 5.1), and in most cases infusions should be initiated slowly (section 7). The hypotensive effects of propofol are often more pronounced in the elderly, in whom clearance of propofol is decreased compared with younger individuals (section 3.3.1); elderly recipients of the drug (aged >55 years) may therefore require a reduced infusion rate (section 7). As with other sedative agents, propofol reduced mean intracranial pressure and maintained mean cerebral perfusion pressure in clinical trials of patients after head trauma (section 4.3).
Several clinical trials have compared propofol with midazolam in patients requiring sedation for general medical conditions, after general or cardiac surgery and following general trauma or head injuries (sections 4.1, 4.2 and 4.3). The quality of sedation achieved with propofol was at least as good as that achieved with midazolam, and in almost all studies the rate of recovery (time to spontaneous ventilation or time to extubation) was significantly faster with propofol (sections 4.1.2 and 4.2).
The faster time to recovery with propofol enables a greater predictability of recovery and easier dosage titration than that observed with midazolam (sections 4.1.2 and 4.2). These qualities have several benefits for the care of the critically ill. A rapid emergence from sedation is particularly beneficial for patients requiring frequent neurological assessment or undergoing short-term procedures, such as physiotherapy, where alterations in the depth of sedation are required.[169] In patients after cardiac surgery, rapid recovery can lead to early mobilisation, better pulmonary function and improved haemodynamics compared with longer recovery times.[167] However, these effects have not yet been shown to produce an improved clinical outcome.[167] Early extubation was shown to lead to earlier discharge from the ICU in a pooled analysis of ten trials comparing early versus late extubation after cardiac surgery.[172] Furthermore, total ICU costs were reduced as a result of early extubation (1–6 hours after the start of sedation) leading to earlier ICU discharge compared with late extubation (12–22 hours after the start of sedation) [section 6].[164]
Since the previous review of propofol in Drugs,[1] more data have become available on the use of the drug for long-term sedation. The shorter times to recovery and extubation in critically ill patients sedated for periods of >72 hours with propofol compared with midazolam was generally more marked than the time differences to recovery observed between the two agents after shorter-duration infusions (section 4.1.2). These studies did not specifically exclude patients with renal or hepatic impairment, who are more likely to experience accumulation of midazolam.
Over the past decade, cost has become a more important factor in choosing a sedative agent.[173] Propofol demonstrated a cost advantage over midazolam in several cost analyses because of a faster time to extubation and, in most cases, an earlier discharge from the ICU (section 6). Despite the higher acquisition cost of propofol, the shorter time spent in the ICU reduced total costs over the short term (approximately <3 days) compared with midazolam. However, in three of four pharmacoeconomic studies, this cost advantage was reduced and eventually disappeared as the period of sedation increased (section 6).
Propofol is generally well tolerated, but hypotension may result from its cardiovascular depressant effects (26% of patients; section 5.1). Hyperlipidaemia is associated with long-term infusions of propofol (>3 days) as a result of the lipid vehicle of the formulation (section 2.5). Patients receiving infusions of >3 days’ duration should have their lipid profiles closely monitored and the calorific value of concomitant parenteral nutrition reduced accordingly (section 7). 2% propofol can be considered when prolonged sedation is indicated. The lipid emulsion also creates a medium for microbial growth (section 5.3), and strict aseptic technique is required when handling the drug, including those formulations containing bacteriostatic or antimicrobial agents. One of the generic formulations of propofol contains sodium metabisulphite (0.25 mg/mL) to retard the growth rate of microorganisms.[174] However, in some patients, allergic reactions to sodium metabisulphite have occurred, more particularly in those with asthma.[174] In some patients receiving higher than recommended dosages of propofol (>5 mg/kg/h) over extended periods (>58 hours), an apparent propofol-infusion syndrome has developed, which can lead to myocardial failure and death (section 5.1.1). For this reason, clinical practice guidelines recommend that patients receiving propofol be monitored for unexplained metabolic acidosis or arrhythmias and, if very high-dose sedation is indicated, patients with escalating vasopressor or inotrope requirements or cardiac failure should receive alternative sedative agents.[165]
Although a number of advantages associated with rapid recovery have been shown in the clinical setting, further data on the clinical relevance of the shorter time to recovery with propofol compared with midazolam are awaited with interest. In addition, a large comparative study of propofol and the new, potent α2-adrenoceptor agonist dexmedetomidine is needed. Dexmedetomidine has demonstrated sedative, analgesic and anxiolytic effects in patients after surgery.[57] In the one small, comparative study with propofol, time to recovery was rapid with both propofol and dexmedetomidine (table IV), but patients receiving propofol required 3-fold more analgesia than those receiving dexmedetomidine (p = 0.004).[57]
In conclusion, the efficacy of propofol in the sedation of adults in the ICU is well established, and clinical trials have demonstrated a similar quality of sedation to midazolam. Because of a rapid distribution and clearance, the duration of action of propofol is short and recovery is rapid. Emergence from sedation is more rapid with propofol than with midazolam, even after long-term administration (>72 hours), which enables better control of the depth of sedation in response to titration and more predictable recovery times. Thus, for the ICU sedation of adults in a variety of clinical settings, propofol provides effective sedation with a more rapid and predictable emergence time than midazolam.
References
Fulton B, Sorkin EM. Propofol.: an overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs 1995 Oct; 50(4): 636–57
Thompson KA, Goodale DB. The recent development of propofol (DIPRIVAN). Intensive Care Med 2000; 26(Suppl. 4): S400–4
Diprivan 1% for I.V. administration: professional information brochure. Wilmington (DE): AstraZeneca, 2001
Mirenda J, Broyles G. Propofol as used for sedation in ICU. Chest 1995 Aug; 108: 539–48
Whitehead C, Sanders LD, Oldroyd G, et al. The subjective effects of low-dose propofol: a double-blind study to evaluate dimensions of sedation and consciousness with low-dose propofol. Anaesthesia 1994; 49: 490–6
Karski JM, Teasdale SJ, Boylan J, et al. Propofol for continuous intravenous sedation after aortocoronary bypass graft surgery: dose finding study [abstract]. Can J Anaesth 1994; 41(5 Suppl.): A17
O’Connor M, Stow P, Mortimer A, et al. Propofol to provide sedation after coronary artery bypass surgery: a comparison of two fixed rate infusion regimens. Acta Anaesthesiol Belg 1992; 43: 235–41
Aitkenhead AR, Willatts SM, Park GR, et al. Comparison of propofol and midazolam for sedation in critically ill patients. Lancet 1989 Sep 23; 2(8665): 704–9
Barrientos-Vega R, Mar Sanchez-Soria M, Morales-Garcia C, et al. Prolonged sedation of critically ill patients with midazolam or propofol: impact on weaning and costs. Crit Care Med 1997 Jan; 25(1): 33–40
Beyer R, Seyde WC. Propofol versus midazolam: long-term sedation in the intensive care unit [in German]. Anaesthesist 1992 Jun; 41(6): 335–41
Boyd O, Mackay CJ, Rushmer F, et al. Propofol or midazolam for short-term alterations in sedation. Can J Anaesth 1993 Dec; 40(12): 1142–7
Chamorro C, de Latorre FJ, Montero A, et al. Comparative study of propofol versus midazolam in the sedation of critically ill patients: results of a prospective, randomized, multicenter trial. Crit Care Med 1996; 24(6): 932–9
Früh B. A comparison of propofol and midazolam for long-term sedation of ventilated patients: a cross-over study. J Drug Dev 1989; 2Suppl. 2: 45–7
Weinbroum AA, Halpern P, Rudick V, et al. Midazolam versus propofol for long-term sedation in the ICU: a randomized prospective comparison. Intensive Care Med 1997 Dec; 23(12): 1258–63
Wolfs C, Kimbimbi P, Colin L, et al. A comparison of propofol/ fentanyl and midazolam/fentanyl for ICU sedation after abdominal surgery. J Drug Dev 1991 Oct; 4 Suppl. 3: 69–71
Grounds RM, Lalor JM, Lumley J, et al. Propofol infusion for sedation in the intensive care unit: preliminary report. BMJ 1987 Feb 14; 294: 397–400
Roekaerts PM, Huygen FJ, de Lange S. Infusion of propofol versus midazolam for sedation in the intensive care unit following coronary artery surgery. J Cardiothorac Vasc Anesth 1993 Apr; 7(2): 142–7
Snellen F, Lauwers P, Demeyere R, et al. The use of midazolam versus propofol for short-term sedation following coronary artery bypass grafting. Intensive Care Med 1990; 16(5): 312–6
Carrasco G, Cabré L, Sobrepere G, et al. Synergistic sedation with propofol and midazolam in intensive care patients after coronary artery bypass grafting. Crit Care Med 1998 May; 26(5): 844–51
McMurray TJ, Collier PS, Carson IW, et al. Propofol sedation after open heart surgery: a clinical and pharmacokinetic study. Anaesthesia 1990 Apr; 45(4): 322–6
Barr J, Egan TD, Sandoval NF, et al. Propofol dosing regimens for ICU sedation based upon an integrated pharmacokinetic-pharmacodynamic model. Anesthesiology 2001 Aug; 95(2): 324–33
McMurray TJ, Johnston JR, Milligan KR, et al. Diprifusor TCI for sedation of ventilated adult ICU patients: target blood propofol concentration settings [poster]. Presented at the 22nd International Symposium of Intensive Care and Emergency Medicine; 2002 Mar 19–22; Brussels
Newman LH, McDonald JC, Wallace PGM, et al. Propofol infusion for sedation in the intensive care unit [letter]. BMJ 1987; 294: 970–1
Higgins TL, Yared J-P, Estafanous FG, et al. Propofol versus midazolam for intensive care unit sedation after coronary artery bypass grafting. Crit Care Med 1994 Sep; 22(9): 1415–23
Ronan KP, Gallagher TJ, George B, et al. Comparison of propofol and midazolam for sedation in intensive care unit patients. Crit Care Med 1995 Feb; 23(2): 286–93
Milne SE, James KS, Nimmo S, et al. Oxygen consumption after hypothermic cardiopulmonary bypass: the effect of continuing a propofol infusion postoperatively. J Cardiothorac Vasc Anesth 2002; 16(1): 32–6
Kress JP, O’Connor MF, Pohlman AS, et al. Sedation of critically ill patients during mechanical ventilation: a comparison of propofol and midazolam. Am J Respir Crit Care Med 1996 Mar; 153: 1012–8
Langley MS, Heel RC. Propofol: a review of its pharmacodynamic and pharmacokinetic properties and use as an intravenous anaesthetic. Drugs 1988; 35: 334–72
Pedersen CM. The effect of sedation with propofol on postoperative bronchoconstriction in patients with hyperreactive airway disease. Intensive Care Med 1992 Mar; 18: 45–6
Conti G, Ferretti A, Tellan G, et al. Propofol induces bronchodilation in a patient mechanically ventilated for status asthmaticus [letter]. Intensive Care Med 1993 Jul; 19: 305
Conti G, Dell’Utri D, Vilardi V, et al. Propofol induces bronchodilation in mechanically ventilated chronic obstructive pulmonary disease (COPD) patients. Acta Anaesthesiol Scand 1993; 37: 105–9
Farling PA, Johnston JR, Coppel DL. Propofol infusion for sedation of patients with head injury in intensive care: a preliminary report. Anaesthesia 1989 Mar; 44(3): 222–6
Farling PA, Johnston JR, Coppel DL. Propofol infusion compared with morphine and midazolam bolus doses for sedation of patients with severe head injuries in the intensive care unit. J Drug Dev 1989; 2 Suppl. 2: 97–8
Vezzani A, Barbagallo M, Furlan A, et al. Neurological assessment and ICP control in severe head injury: use of propofol as a short-acting sedative agent. J Drug Dev 1991; 4 Suppl. 3: 114–5
Mergaert C, Herregods L, Rolly G, et al. The effect of a 24-h propofol or fentanyl sedation on intracranial pressure [abstract]. Eur J Anaesthesiol 1991; 8: 324–5
Weinstabl C, Mayer N, Plattner H, et al. Impact of propofol on intracranial dynamics in head trauma ICU patients [abstract no. A1217]. Anesthesiology 1990 Sep; 73 (Suppl. 3A)
Boyle WA, Shear JM, White PF, et al. Long-term sedative infusion in the intensive care unit: propofol versus midazolam. J Drug Dev 1991 Oct; 4Suppl. 3: 43–5
Foster SJ, Buckley PM. A retrospective review of two years’ experience with propofol in one intensive care unit. J Drug Dev 1989; 2 Suppl. 2: 73–4
Buckley PM. Propofol in patients needing long-term sedation in intensive care: an assessment of the development of tolerance. A pilot study. Intensive Care Med 1997 Sep; 23(9): 969–74
Cook S, Palma O. Propofol as a sole agent for prolonged infusion in intensive care. J Drug Dev 1989; 2 Suppl. 2: 65–7
Carrasco G, Molina R, Costa J, et al. Propofol vs midazolam in short-, medium-, and long-term sedation of critically ill patients; a cost-benefit analysis. Chest 1993; 103(2): 557–64
McLeod G, Dick J, Wallis C, et al. Propofol 2% in critically ill patients: effect on lipids. Crit Care Med 1997 Dec; 25(12): 1976–81
Barrientos-Vega R, Sánchez-Soria MM, Morales-Garcia C, et al. Pharmacoeconomic assessment of propofol 2% used for prolonged sedation. Crit Care Med 2001 Feb; 29(2): 317–22
Plunkett JJ, Reeves JD, Ngo L, et al. Urine and plasma catecholamine and cortisol concentrations after myocardial revascularization: modulation by continuous sedation. Anesthesiology 1997 Apr; 86(4): 785–96
Heller A, Heller S, Blecken S, et al. Effects of intravenous anesthetics on bacterial elimination in human blood in vitro. Acta Anaesthesiol Scand 1998; 42: 518–26
Mikawa K, Akamatsu H, Nishina K, et al. Propofol inhibits human neutrophil functions. Anesth Analg 1998; 87: 695–700
Galley HF, Dubbels AM, Webster NR. The effect of midazolam and propofol on interleukin-8 from human polymorphonuclear leukocytes. Anesth Analg 1998; 86: 1289–93
Pirttikangas C-O, Perttilä J, Salo M. Propofol emulsion reduces proliferative responses of lymphocytes from intensive care patients. Intensive Care Med 1993 Jul; 19: 299–302
Kelbel I, Weiss M. Anaesthetics and immune function. Curr Opin Anaesthesiol 2001; 14(6): 685–91
Barr J, Egan T, Feeley T, et al. Depth of sedation vs. propofol concentration in mechanically ventilated ICU patients [abstract no. A313]. Anesthesiology 1992 Sep; 77 Suppl. 3A
Sorbara C, Armellin G, Bonato A, et al. Postoperative sedation with propofol infusion: haemodynamics and pharmacokinetics. Clin Drug Invest 1998; 16(6): 431–9
Wang S-H, Hsu K-Y, Uang Y-S. Long-term continuous infusion of propofol as a means of sedation for patients in intensive care unit: relationship between dosage and serum concentration. Acta Anaesthesiol Sin 1998 Jun; 36(2): 93–8
Ramsay MAE, Savege TM, Simpson BRJ, et al. Controlled sedation with alphaxalone-alphadolone. BMJ 1974; 2: 656–9
Angelini G, Ketzler JT, Coursin DB. Use of propofol and other nonbenzodiazepine sedatives in the intensive care unit. Crit Care Clin 2001 Oct; 17(4): 863–80
Telci I, Denkel T, Esen F, et al. Cardiocirculatory effects of propofol in acute respiratory failure: a clinical trial. J Drug Dev 1991 Oct; 4 Suppl. 3: 93–4
Searle NR, Côté S, Taillefer J, et al. Propofol or midazolam for sedation and early extubation following cardiac surgery. Can J Anaesth 1997 Jun; 44(6): 629–35
Venn RM, Grounds RM. Comparison between dexmedetomidine and propofol for sedation in the intensive care unit: patient and clinician perceptions. Br J Anaesth 2001 Nov; 87(5): 684–90
Sandiumenge Camps A, Sanchez-Izquierdo Riera JA, Toral Vazquez D, et al. Midazolam and 2% propofol in long-term sedation of traumatized critically ill patients: efficacy and safety comparison. Crit Care Med 2000 Nov; 28(11): 3612–9
Ewart MC, Yau KW, Morgan M. 2% Propofol for sedation in the intensive care unit: a feasibility study. Anaesthesia 1992 Feb; 47(2): 146–8
Hammarén E, Scheinin M, Hynynen M. Effect of low-dose propofol infusion on total-body oxygen consumption after coronary artery surgery. J Cardiothorac Vasc Anesth 1999 Apr; 13(2): 154–9
Cohen D, Horiuchi K, Kemper M, et al. Modulating effects of propofol on metabolic and cardiopulmonary responses to stressful intensive care unit procedures. Crit Care Med 1996; 24(4): 612–7
McMurray TC. Propofol for sedation following cardiac surgery. J Drug Dev 1991; 4 Suppl. 3: 51–8
Barr J. Propofol: a new drug for sedation in the intensive care unit. Int Anesthesiol Clin 1995 Winter; 33(1): 131–54
Hall RI, Sandham D, Cardinal P, et al. Propofol vs midazolam for ICU sedation: a Canadian multicenter randomized trial. Chest 2001 Apr; 119(4): 1151–9
Khamiees M, Amoateng-Adjepong Y, Manthous CA. Propofol infusion is associated with a higher rapid shallow breathing index in patients preparing to wean from mechanical ventilation. Respir Care 2002 Feb; 47(2): 150–3
Shafer A. Complications of sedation with midazolam in the intensive care unit and a comparison with other sedative regimens. Crit Care Med 1998 May; 26(5): 947–56
Degaugue C, Dupuis A. A study to compare the use of propofol and midazolam for the sedation of patients with acute respiratory failure. J Drug Dev 1991 Oct; 4 Suppl. 3: 95–7
Stewart L, Bullock R, Rafferty C, et al. Propofol sedation in severe head injury fails to control high ICP, but reduces brain metabolism. Acta Neurochir 1994; 60 Suppl.: 544–6
Matta BF, Risdall J, Menon DK, et al. The effect of propofol on cerebral autoregulation after head injury: a preliminary report. Br J Anaesth 1997 May; 78 Suppl. 1: 72
Kishimoto T, Kadoya C, Sneyd R, et al. Topographic electroencephalogram of propofol-induced conscious sedation. Clin Pharmacol Ther 1995; 58: 666–74
Theilen HJ, Adam S, Kuhlisch E, et al. Progressive electroencephalogram frequency deceleration despite constant depth of propofol-induced sedation. Crit Care Med 2002 Aug; 30(8): 1787–93
Sneyd JR, Samra SK, Davidson B, et al. Electrophysiologic effects of propofol sedation. Anesth Analg 1994; 79: 1151–8
Magarey JM. Propofol or midazolam — which is best for the sedation of adult ventilated patients in intensive care units? A systematic review. Aust Crit Care 2001 Nov; 14(4): 147–54
Treggiari-Venzi M, Borgeat A, Fuchs-Buder T, et al. Overnight sedation with midazolam or propofol in the ICU: effects on sleep quality, anxiety and depression. Intensive Care Med 1996 Nov; 22(11): 1186–90
McLeod G, Wallis C, Dick J, et al. Use of 2% propofol to produce diurnal sedation in critically ill patients. Intensive Care Med 1997 Apr; 23(4): 428–34
Polster MR, Gray PA, O’Sullivan G, et al. Comparison of the sedative and amnesic effects of midazolam and propofol. Br J Anaesth 1993; 70: 612–6
Montanini S, Pratico C, Tufano R, et al. Propofol for sedation in the intensive care unit: comparative evaluation of 1% and 2% formulations. Br J Intensive Care 1999; 9(4): 110–4
Leisure GS, O’Flaherty J, Green L, et al. Propofol and postoperative pancreatitis. Anesthesiology 1996; 84(1): 224–7
Kumar AN, Schwartz DE, Lim KG. Propofol-induced pancreatitis: recurrence of pancreatitis after rechallenge. Chest 1999; 115: 1198–9
Possidente CJ, Rogers FB, Osler TM, et al. Elevated pancreatic enzymes after extended propofol therapy. Pharmacotherapy 1998; 18(3): 653–5
Wingfield TW. Pancreatitis after propofol administration: is there a relationship? Anesthesiology 1996; 84(1): 236
Piper SN, Kumle B, Maleck WH, et al. Effects of postoperative sedation with propofol and midazolam on pancreatic function assessed by pancreatitis-associated protein. Anaesthesia 2001 Sep; 56(9): 836–40
Hall RI, MacLaren C, Smith MS, et al. Light versus heavy sedation after cardiac surgery: myocardial ischemia and the stress response. Anesth Analg 1997 Nov; 85: 971–8
Cox C, McLeod G, Wallis C, et al. Use of 2% propofol to produce night sedation in critically ill patients: effect on hormones. Br J Anaesth 1995 May; 74 Suppl. 1: 114
Lee T-L, Ang SBL, Dambisya YM, et al. The effect of propofol on human gastric and colonic muscle contractions. Anesth Analg 1999 Nov; 89(5): 1246–9
Freye E, Sundermann S, Wilder-Smith OHG. No inhibition of gastro-intestinal propulsion after propofol- or propofol/ ketamine-N2O/O2 anaesthesia: a comparison of gastro-caecal transit after isoflurane anaesthesia. Acta Anaesthesiol Scand 1998 Jul; 42(6): 664–9
Devlin EG, Clarke RSJ, Mirakhur RK, et al. Effect of four i.v. induction agents on T-lymphocyte proliferations to PHA in vitro. Br J Anaesth 1994; 73: 315–7
O’Donnell CA, O’Donnell NG, McSharry CP, et al. Comparison of the effects of propofol and thiopentone on white blood cell function. Hum Exp Toxicol 1991; 10(6): 483
Helmy SAK, Wahby MAM, El-Nawaway M. The effect of anaesthesia and surgery on plasma cytokine production. Anaesthesia 1999; 54(8): 733–8
Helmy SAK, Al-Attiyah RJ. The immunomodulatory effects of prolonged intravenous infusion of propofol versus midazolam in critically ill surgical patients. Anaesthesia 2001; 56: 4–8
Abraham E, Papadakos PJ, Tharratt RS, et al. Effects of propofol containing EDTA on mineral metabolism in medical ICU patients with pulmonary dysfunction. Intensive Care Med 2000; 26Suppl. 4: S422–32
Herr DL, Kelly K, Hall JB, et al. Safety and efficacy of propofol with EDTA when used for sedation of surgical intensive care unit patients. Intensive Care Med 2000; 26Suppl. 4: S452–62
Wahr J, Vender J, Gilbert HC, et al. Effect of propofol with and without EDTA on haemodynamics and calcium and magnesium homeostasis during and after cardiac surgery. Intensive Care Med 2000; 26 Suppl.: 443–51
Higgins TL, Murray M, Kett DH, et al. Trace element homeostasis during continuous sedation with propofol containing EDTA versus other sedatives in critically ill patients. Intensive Care Med 2000; 26Suppl. 4: S413–21
Zaloga GP, Youngs E, Teres D. Propofol-containing sedatives increase levels of parathyroid hormone. Intensive Care Med 2000; 26 Suppl.: 405–12
Kanto J, Gepts E. Pharmacokinetic implications for the clinical use of propofol. Clin Pharmacokinet 1989; 17(5): 308–26
Frenkel C, Schüttler J, Ihmsen H, et al. Pharmacokinetics and pharmacodynamics of propofol/alfentanil infusions for sedation in ICU patients. Intensive Care Med 1995 Dec; 21(12): 981–8
Albanese J, Martin C, Lacarelle B, et al. Pharmacokinetics of long-term propofol infusion used for sedation in ICU patients. Anesthesiology 1990; 73(2): 214–7
Bailie GR, Cockshott ID, Douglas EJ, et al. Pharmacokinetics of propofol during and after long-term continuous infusion for maintenance of sedation in ICU patients. Br J Anaesth 1992 May; 68(5): 486–91
Cockshott ID. The pharmacokinetics of propofol in the ICU patient. J Drug Dev 1991 Oct; 4 Suppl. 3: 29–36
AstraZeneca. Diprivan global prescribing information [online]. Available from URL: http://anaesthesia-az.com [Accessed 2002 Nov 1]
Zamacona MK, Suárez E, Aguilera L, et al. Serum protein binding of propofol in critically ill patients. Acta Anaesthesiol Scand 1997 Nov; 41: 1267–72
Simons PJ, Cockshott ID, Douglas EJ, et al. Disposition in male volunteers of a subanaesthetic intravenous dose of an oil in water emulsion of 14C-propofol. Xenobiotica 1988; 4: 429–40
Van Brandt N, Hantson P, Horsmans Y, et al. Effect of enteral versus parenteral feeding on hepatic blood flow and steady state propofol pharmacokinetics in ICU patients. Intensive Care Med 1998 Aug; 24(8): 795–800
Kirkpatrick T, Cockshott ID, Douglas EJ, et al. Pharmacokinetics of propofol (Diprivan) in elderly patients. Br J Anaesth 1988; 60: 146–50
Shafer A, Doze VA, Shafer SL, et al. Pharmacokinetics and pharmacodynamics of propofol infusions during general anesthesia. Anesthesiology 1988; 69: 348–56
Eddleston JM, Pollard BJ, Blades JF, et al. The use of propofol for sedation of critically ill patients undergoing haemodiafiltration. Intensive Care Med 1995 Apr; 21: 342–7
Barr J, Zaloga GP, Haupt MT, et al. Cation metabolism during propofol sedation with and without EDTA in patients with impaired renal function. Intensive Care Med 2000; 26Suppl. 4: S433–42
Ibrahim AE, Park S, Feldman J, et al. No effect of parecoxib, a parenteral COX-2 specific inhibitor, on the disposition of propofol. Anaesth Intensive Care 2002 Apr; 30: 247
McCollam JS, O’Neil MG, Norcross ED, et al. Continuous infusions of lorazepam, midazolam, and propofol for sedation of the critically ill surgery trauma patient: a prospective, randomized comparison. Crit Care Med 1999 Nov; 27(11): 2454–8
Millane TA, Bennett ED, Grounds RM. Isoflurane and propofol for long-term sedation in the intensive care unit: a crossover study. Anaesthesia 1992 Sep; 47(9): 768–74
O’Connor M, Stow P, Mortimer A, et al. Propofol to provide sedation after coronary artery by-pass surgery: a comparison of three fixed-rate infusion regimens. J Drug Dev 1989; 2 Suppl. 2: 135–7
Vandenberghe J, Rucquoi M, Camu F. Propofol sedation for controlled ventilation of post-operative aortic surgery patients: an evaluation of haemodynamics and sedation. J Drug Dev 1991; 4 Suppl. 3: 65–6
Beller JP, Pottecher T, Lugnier A, et al. Prolonged sedation with propofol in ICU patients: recovery and blood concentration changes during periodic interruptions in infusion. Br J Anaesth 1988; 61: 583–8
d’Athis F, Chardon P, Mathieu-Daudé JC, et al. Propofol for sedation in the intensive care unit. J Drug Dev 1989; 2Suppl. 2: 61–4
DuGres B, Flamens C. A comparison of propofol and midazolam infusion for post operative sedation after cardiac surgery [abstract]. J Cardiothorac Anesth 1990; 4(6 Suppl. 3): 101
Nollet G, Verbeke J. Comparison of propofol and alfentanil as sedative agents after coronary artery by-pass graft. J Drug Dev 1991; 4 Suppl. 3: 62–4
Leino K, Nunes S, Valta P, et al. The effect of sedation on weaning following coronary artery bypass grafting: propofol versus oxycodone-thiopental. Acta Anaesthesiol Scand 2000 Apr; 44(4): 369–77
Wahr JA, Plunkett JJ, Ramsay JG, et al. Cardiovascular responses during sedation after coronary revascularization. Incidence of myocardial ischemia and hemodynamic episodes with propofol versus midazolam. Anesthesiology 1996; 84(6): 1350–60
Mirski MA, Muffelman B, Ulatowski JA, et al. Sedation for the critically ill neurologic patient. Crit Care Med 1995; 23(12): 2038–53
Pearson K, Kruse G, Demetrion E. Sedation of patients with severe head injury. a randomized, prospective comparison of propofol versus morphine and barbiturates [abstract no. A248]. Anesthesiology 1991; 75 (3A)
Kelly DF, Goodale DB, Williams J, et al. Propofol in the treatment of moderate and severe head injury: a randomized, prospective double-blinded pilot trial. J Neurosurg 1999; 90: 1042–52
Smith M. Postoperative neurosurgical care. Curr Anaesth Crit Care 1994; 5(1): 29–35
Dewandre J, Van Bos RJ, Van Hemelrijck J, et al. Comparison of the 2% and 1% formulations of propofol during anaesthesia for craniotomy. Anaesthesia 1994; 49: 8–12
Escarment J, Donne X, Palmier B, et al. Quality of sedation and neurologic evaluation following surgery of the posterior cranial fossa: the importance of propofol [in French]. Cah Anesthesiol 1992; 40(1): 29–35
Clarke TNS. Propofol compared with midazolam for sedation following prolonged neurosurgery. J Drug Dev 1991; 4 Suppl. 3: 108–9
Löffler WH, Wallner F, Fischer J, et al. Comparison of electroencephalography, cerebral perfusion pressure, and recovery times following propofol of methohexital sedation in neurosurgical patients. J Clin Monit 1993; 9(2): 146–7
MacKenzie SJ, Kapadia F, Grant IS. Propofol infusion for control of status epilepticus. Anaesthesia 1990; 45: 1043–5
McBurney JW, Teiken PJ, Moon MR. Propofol for treating status epilepticus. J Epilepsy 1994; 7(1): 21–2
Natalè E, Mattaliano A, Alia G, et al. Propofol in treatment of status epilepticus: report of four cases successfully treated [abstract]. Epilepsia 1993; 34 Suppl. 2: 124–5
Rousseff R, Bojinov St, Platikanov W. Propofol in intractable status epilepticus. Epilepsia 1996; 37 Suppl. 4: 74–5
Wood PR, Browne GPR, Pugh S. Propofol infusion for the treatment of status epilepticus [letter]. Lancet 1988 Feb; 1(8583): 480–1
Yanny HF, Christmas D. Propofol infusions for status epilepticus [letter]. Anaesthesia 1988; 43(6): 514
Saeed AB, Javidan M. Propofol for treatment of non convulsive status epilepticus in intensive care unit [abstract]. Crit Care Med 2000 Dec; 28 Suppl.: 98
Fox FL, Bostwick JM. Propofol sedation of refractory delirious mania. Psychosomatics 1997; 38(3): 288–90
Ermakov S, Hoyt J, Crippen D. Conscious sedation with propofol in patients with delirium tremens [abstract]. Crit Care Med 1995; 23(1): A68
Stiebel VG, Crippen D, Ermakov S. Treatment of delirium tremens with continuous propofol infusion [abstract]. Psychosomatics 1994; 35(2): 193
Borgeat A, Popovis V, Schwander D. Efficiency in a continuous infusion of propofol in a patient with tetanus. Crit Care Med 1991; 19(2): 295–7
Borgeat A, Dessibourg C, Rochani M, et al. Sedation by propofol in tetanus — is it a muscular relaxant? Intensive Care Med 1991; 17: 427–9
Orko R, Rosenberg PH, Himberg J-J. Intravenous infusion of midazolam, propofol and vecuronium in a patient with severe tetanus. Acta Anaesthesiol Scand 1988 Oct; 32(7): 590–2
Parke TJ, Stevens JE, Rice ASC, et al. Metabolic acidosis and fatal myocardial failure after propofol infusion in children: five case reports. BMJ 1992; 305(6854): 613–6
Bray RJ. Propofol infusion syndrome in children. Paediatr Anaesth 1998; 8: 491–9
Kelly DF. Propofol-infusion syndrome. J Neurosurg 2001; 95: 925–6
Cremer OL, Moons KGM, Bouman EAC, et al. Long-term propofol infusion and cardiac failure in adult head-injured patients [letter]. Lancet 2001 Jan 13; 357(9250): 117–8
Perrier ND, Baerga-Varela Y, Murray MJ. Death related to propofol use in an adult patient. Crit Care Med 2000 Aug; 28(8): 3071–4
Sutherland MJ, Burt P. Propofol and seizures. Anaesth Intensive Care 1994 Dec; 22: 733–7
Collier C, Kelly K. Propofol and convulsions: the evidence mounts. Anaesth Intensive Care 1991 Nov; 19: 573–5
McManus KF. Convulsion after propofol enflurane [letter]. Anaesth Intensive Care 1992 May; 20: 245
Harrigan PWJ, Browne SM, Quail AW. Multiple seizures following re-exposure to propofol. Anaesth Intensive Care 1996 Apr; 24: 261–4
Bennett SN, McNeil MM, Bland LA, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med 1995; 333(3): 147–54
Webb SAR, Roberts B, Breheny FX, et al. Contamination of propofol infusions in the intensive care unit: incidence and clinical significance. Anaesth Intensive Care 1998 Apr; 26(2): 162–4
Bach A, Motsch J, Schmidt H, et al. In-use contamination of propofol. A clinical study. Eur J Anaesthesiol 1997 Mar; 14: 178–83
Marinella MA. Propofol for sedation in the intensive care unit: essentials for the clinician. Respir Med 1997 Oct; 91(9): 505–10
Bodenham A, Culank LS, Park GR. Propofol infusion and green urine [letter]. Lancet 1987; 11: 740
Ananthanarayan C, Fisher JA. Why was the urine green? [letter]. Can J Anaesth 1995; 42(1): 87–8
Motsch J, Schmidt H, Bach A, et al. Long-term sedation with propofol and green discolouration of the liver. Eur J Anaesthesiol 1994 Nov; 11(6): 499–502
Callander CC, Thomas JS, Evans CJ. Propofol and the colour green [letter]. Anaesthesia 1989; 44: 82
McHale SP, Konieczko K. Anaphylactoid reaction to propofol. Anaesthesia 1992; 47: 864–5
Laxenaire M-C, Mata-Bermejo E, Moneret-Vautrin DA, et al. Life-threatening anaphylactoid reactions to propofol (Diprivan). Anesthesiology 1992; 77: 275–80
Anis AH, Wang X, Leon H, et al. Economic evaluation of propofol for sedation of patients admitted to intensive care units. Anesthesiology 2002 Jan; 96(1): 196–201
Manley NM, Fitzpatrick RW, Long T, et al. A cost analysis of alfentanil+propofol vs morphine+midazolam for the sedation of critically ill patients. Pharmacoeconomics 1997 Aug; 12 (2 Pt 2): 247–55
Sherry KM, McNamara J, Brown JS, et al. An economic evaluation of propofol/fentanyl compared with midazolam/ fentanyl on recovery in the ICU following cardiac surgery. Anaesthesia 1996 Apr; 51: 312–7
Costa J, Cabré L, Molina R, et al. Cost of ICU sedation: comparison of empirical and controlled sedation methods. Clin Intensive Care 1994; 5(5 Suppl.): 17–21
Cheng DCH, Karski J, Peniston C, et al. Early tracheal extubation after coronary artery bypass graft surgery reduces costs and improves resource use: a prospective randomized controlled trial. Anesthesiology 1996; 85: 1300–10
Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30(1): 119–40
Kang TM. Propofol infusion syndrome in critically ill patients. Ann Pharmacother 2002; 36: 1453–6
Abraham E. Managing sedative agents in common ICU settings. Crit Care Med 2002; 30(1 Suppl. A): S110–3
Young C, Knudsen N, Hilton A, et al. Sedation in the intensive care unit. Crit Care Med 2000 Mar; 28(3): 854–66
Hill L, Bertaccini E, Barr J, et al. ICU sedation: a review of its pharmacology and assessment. J Intensive Care Med 1998; 13(4): 174–83
Radu O, Groth M. Propofol or midazolam for sedation in the ICU: which one is better? Clin Pulmonary Med 2001; 8(5): 303–4
Shapiro BA, Warren J, Egol AB, et al. Practice parameters for intravenous analgesia and sedation for adult patients in the intensive care unit: an executive summary. Crit Care Med 1995 Sep; 23(9): 1596–600
Meade MO, Guyatt G, Butler R, et al. Trials comparing early vs late extubation following cardiovascular surgery. Chest 2001 Dec; 120(6 Suppl.): 445S–53S
Crippen D. High-tech assessment of patient comfort in the intensive care unit: time for a new look. Crit Care Med 2002 Aug; 30(8): 1919–20
Baxter Healthcare Corporation. Propofol: injectable emulsion 1% 10 mg/ml propofol. Prescribing information. Irvine (CA): Baxter Healthcare Corporation, 2002 Jul
Author information
Authors and Affiliations
Corresponding author
Additional information
Use of tradenames is for product identification purposes only and does not imply endorsement
Various sections of the manuscript reviewed by: L. Burry, Departments of Pharmacy and Critical Care, Mt Sinai Hospital, Toronto, ON, Canada; C. Chamorro, Intensive Care Unit, Clinica Puerta de Hierro, Madrid, Spain; D. Drover, Department of Anesthesia, Stanford University Medical Center, Stanford, CA, USA; R. Hall, Department of Anaesthesia, Queen Elizabeth II Health Sciences Centre, Halifax, NS, Canada; S Mehta, Departments of Pharmacy and Critical Care, Mt Sinai Hospital, Toronto, ON, Canada; S. K. Samra, Department of Anesthesiology, University of Michigan Health System, Ann Arbor, MI, USA; N. R. Searle, Department of Anaesthesia, Montreal Heart Institute, Montreal, PQ, Canada.
Data Selection
Sources: Medical literature published in any language since 1980 on propofol, identified using Medline and EMBASE, supplemented by AdisBase (a proprietary database of Adis International). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: Medline search terms were ‘propofol,’ ‘ICU’ or ‘intensive care*’ and ‘sedation’. EMBASE search terms were ‘propofol’, ‘ICU’ or ‘intensive care*’ and ‘sedation’. AdisBase search terms were ‘propofol’, ‘ICU’ or ‘intensive care*’ and ‘sedation’. Searches were last updated 3 February 2003.
Selection: Studies in patients who received propofol for intensive care unit sedation. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: ICU sedation, pharmacodynamics, pharmacokinetics, propofol, therapeutic use.
Rights and permissions
About this article
Cite this article
McKeage, K., Perry, C.M. Propofol. CNS Drugs 17, 235–272 (2003). https://doi.org/10.2165/00023210-200317040-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200317040-00003